Title: Understanding the Tennessee General Notice of Preexisting Condition Exclusion Keywords: Tennessee, General Notice, Preexisting Condition Exclusion, types Introduction: The Tennessee General Notice of Preexisting Condition Exclusion is a vital document that outlines specific regulations regarding the coverage of preexisting medical conditions within the state's insurance industry. This detailed description aims to shed light on its purpose, significance, and any potential types or variations that exist within Tennessee. Definition: The General Notice of Preexisting Condition Exclusion refers to a legal notice that insurance companies in Tennessee provide to policyholders, informing them about the terms and conditions surrounding coverage limitations related to preexisting medical conditions. It aims to ensure transparency and clarity for policyholders when it comes to accessing medical services. Purpose and Significance: The primary purpose of the Tennessee General Notice of Preexisting Condition Exclusion is to protect insurance companies from the potential financial risks associated with insuring individuals who have preexisting medical conditions. By prominently addressing preexisting conditions, insurance companies can establish specific limitations or exclusions from coverage, allowing them to manage costs effectively. Types of Tennessee General Notice of Preexisting Condition Exclusion: 1. Standard Preexisting Condition Exclusion: This type of exclusion refers to a uniform notice provided by insurance companies operating within Tennessee. It outlines the general conditions and limitations applicable to all policies within the state. 2. Carrier-Specific Preexisting Condition Exclusion: Some insurance carriers may have their unique variations of the General Notice of Preexisting Condition Exclusion. These notices may include additional stipulations or specific conditions not covered by the standard notice. It is crucial for policyholders to thoroughly review these carrier-specific exclusions to understand the extent of coverage provided. Key Considerations: 1. Duration: The notice explains the duration for which a preexisting condition may be excluded from coverage. This period varies but typically ranges from six months to a year after the policy's effective date. 2. Grandfathered Plans: The general notice may also highlight the insurance plans that are "grandfathered," meaning they are not subject to the same preexisting condition exclusions. These plans may have more lenient terms regarding coverage for preexisting conditions. 3. Mandatory Renew ability: The notice emphasizes the mandatory renew ability of policies, ensuring that a preexisting condition exclusion cannot extend indefinitely. After the exclusion period expires, coverage for preexisting conditions should be included in subsequent policy renewals. Conclusion: In summary, the Tennessee General Notice of Preexisting Condition Exclusion is a crucial document that governs the coverage limitations and exclusions for policyholders with preexisting medical conditions in the state. It plays a significant role in ensuring transparency, managing financial risks for insurance companies, and providing individuals with a clear understanding of their policy. Policyholders should carefully review this notice and any carrier-specific variations to fully comprehend the extent of coverage for preexisting conditions.
Tennessee General Notice of Preexisting Condition Exclusion
Description
How to fill out Tennessee General Notice Of Preexisting Condition Exclusion?
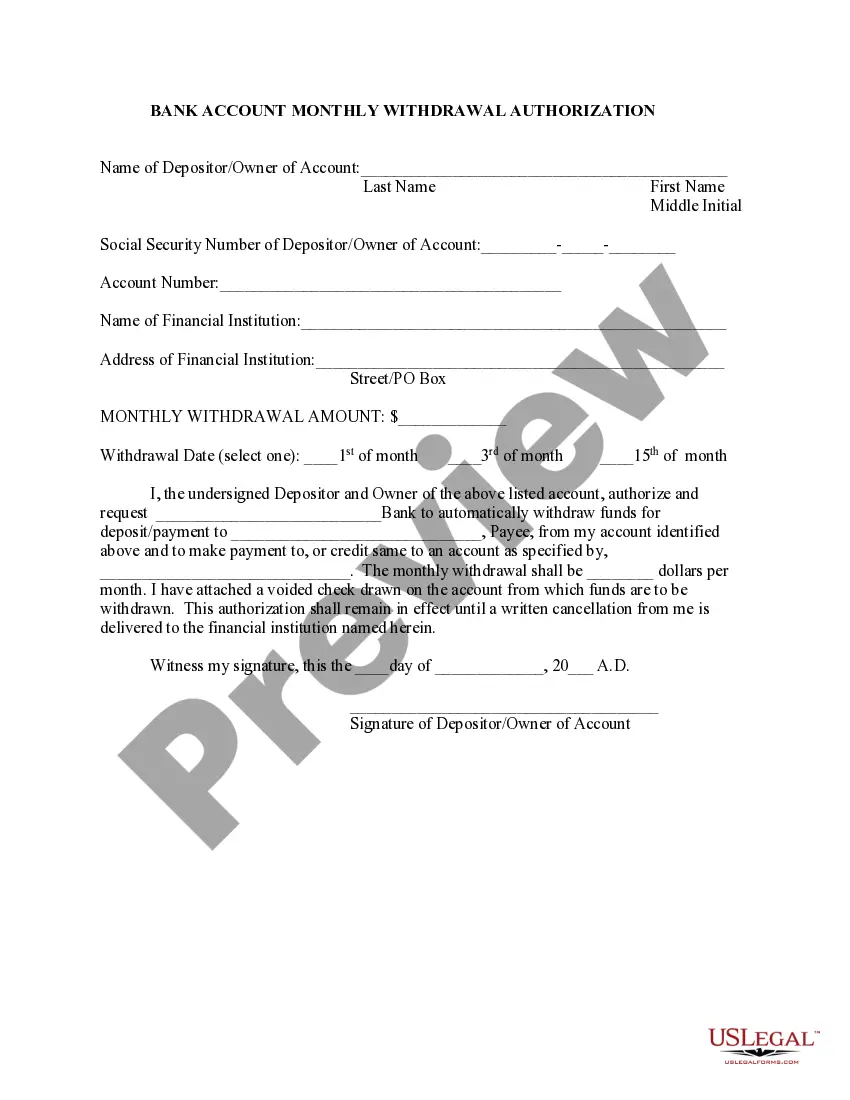
Discovering the right authorized document format can be quite a struggle. Obviously, there are tons of templates available on the net, but how do you discover the authorized develop you need? Use the US Legal Forms site. The service offers a large number of templates, for example the Tennessee General Notice of Preexisting Condition Exclusion, that you can use for business and private needs. Every one of the types are examined by professionals and meet state and federal demands.
In case you are already listed, log in for your profile and click the Acquire key to get the Tennessee General Notice of Preexisting Condition Exclusion. Make use of profile to check from the authorized types you possess ordered previously. Visit the My Forms tab of your own profile and get another version from the document you need.
In case you are a fresh customer of US Legal Forms, here are basic instructions so that you can comply with:
- Initial, be sure you have chosen the appropriate develop to your metropolis/region. You are able to look through the shape making use of the Review key and study the shape outline to make certain this is the best for you.
- When the develop is not going to meet your preferences, make use of the Seach industry to find the proper develop.
- Once you are positive that the shape is suitable, go through the Purchase now key to get the develop.
- Choose the costs strategy you would like and enter in the necessary details. Create your profile and pay money for the order with your PayPal profile or bank card.
- Pick the submit formatting and obtain the authorized document format for your product.
- Complete, modify and print and indicator the obtained Tennessee General Notice of Preexisting Condition Exclusion.
US Legal Forms will be the most significant local library of authorized types for which you can see various document templates. Use the company to obtain expertly-produced papers that comply with state demands.