Tennessee Notice of Special Enrollment Rights, also known as TN USER, is an essential document that ensures residents of Tennessee have access to crucial health insurance coverage during significant life changes. This detailed description aims to shed light on the significance and types of Tennessee Notice of Special Enrollment Rights, providing clarity for individuals seeking information regarding this topic. The Tennessee Notice of Special Enrollment Rights serves as a notification to individuals about their ability to enroll in or modify health insurance coverage outside the regular enrollment period. These special enrollment rights are granted under specific circumstances, allowing individuals to address significant life events that may affect their healthcare coverage needs. By understanding and utilizing the Tennessee Notice of Special Enrollment Rights, individuals gain the opportunity to secure health insurance coverage when they experience qualifying life events. Such events may include marriage, divorce, the birth or adoption of a child, loss of previous health insurance coverage, permanent relocation, changes in employment status, or changes in household size or income. In Tennessee, there are several types of Notice of Special Enrollment Rights depending on the circumstances individuals find themselves in. These types encompass various life events, ensuring that individuals are not left without adequate health coverage during critical periods. The common types of Tennessee Notice of Special Enrollment Rights include: 1. Regular Special Enrollment Period: This type enables individuals to enroll in health insurance coverage or modify their existing coverage during open enrollment periods, allowing them to secure the necessary protection for themselves and their dependents. 2. Qualifying Life Events: Individuals experiencing specific life events, such as marriage, divorce, or the birth or adoption of a child, are eligible for a special enrollment period. This allows them to adjust their health insurance plans accordingly to accommodate the new circumstances. 3. Loss of Previous Coverage: Those who have experienced a loss of previous health insurance coverage, whether due to job loss, eligibility expiration, or loss of dependent status, are granted special enrollment rights. This ensures they can swiftly obtain alternative coverage to maintain uninterrupted healthcare. 4. Permanent Relocation: Individuals who have moved to a different residence within or outside of Tennessee are eligible for a special enrollment period. This allows them to access health insurance coverage specific to their new location, addressing any changes in available options. 5. Changes in Employment Status: Individuals who experience changes in employment status, like leaving a job or starting a new one, may qualify for special enrollment rights. This ensures they can obtain suitable health insurance coverage that meets their evolving needs. 6. Changes in Household Size or Income: Individuals who experience changes in household size or significant fluctuations in income qualify for special enrollment periods. This allows them to adapt their health insurance coverage accordingly, ensuring their plan matches their current situation. It is crucial for residents of Tennessee to familiarize themselves with the Tennessee Notice of Special Enrollment Rights and understand the types of qualifying events that entitle them to these special enrollment periods. This knowledge empowers individuals to make informed decisions about their healthcare coverage during critical times, safeguarding their well-being and that of their loved ones.
Tennessee Notice of Special Enrollment Rights
Description
How to fill out Tennessee Notice Of Special Enrollment Rights?
Choosing the best authorized document format can be a struggle. Of course, there are plenty of templates available online, but how can you obtain the authorized type you require? Make use of the US Legal Forms website. The services gives a large number of templates, such as the Tennessee Notice of Special Enrollment Rights, that can be used for enterprise and personal demands. Each of the varieties are checked out by experts and meet up with federal and state demands.
Should you be already registered, log in to the accounts and click on the Download button to have the Tennessee Notice of Special Enrollment Rights. Utilize your accounts to check with the authorized varieties you might have bought previously. Check out the My Forms tab of your respective accounts and obtain another version of the document you require.
Should you be a whole new customer of US Legal Forms, allow me to share basic recommendations that you can stick to:
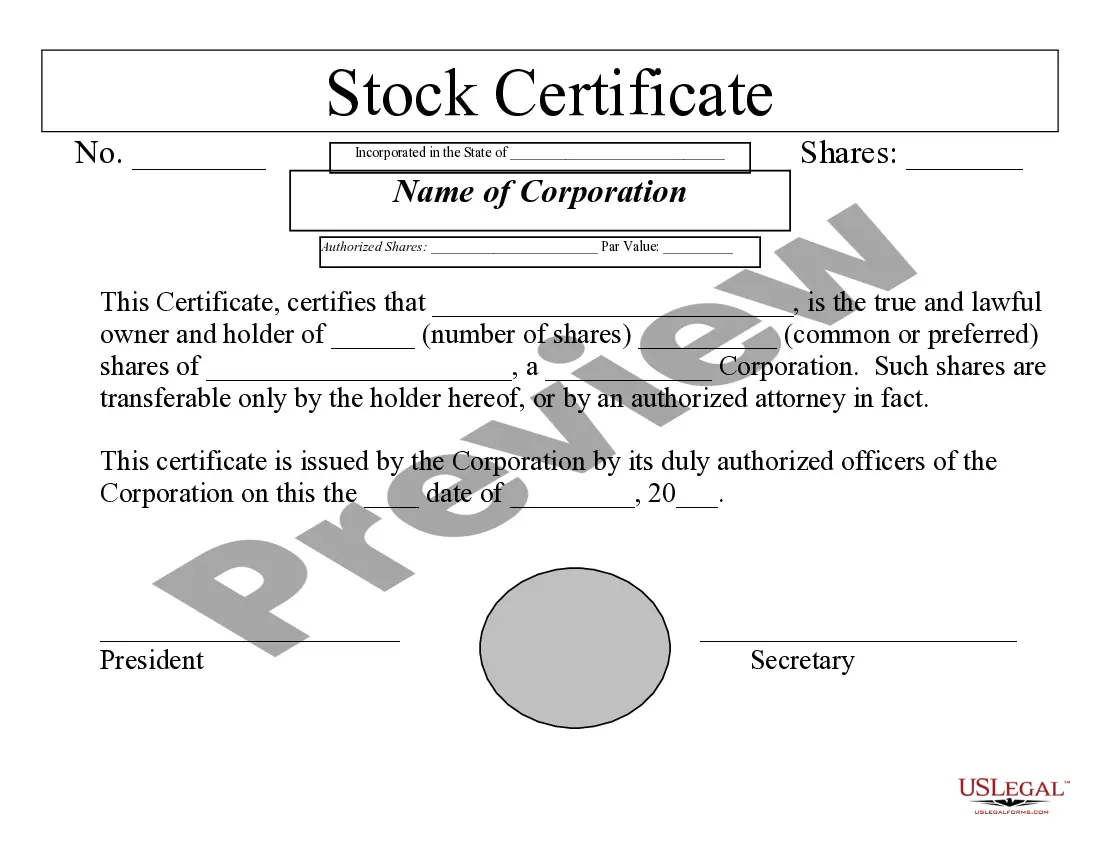
- Initially, be sure you have chosen the correct type for your personal city/region. You are able to examine the form while using Review button and study the form information to make certain it will be the right one for you.
- If the type does not meet up with your needs, utilize the Seach discipline to find the proper type.
- Once you are certain that the form is suitable, select the Buy now button to have the type.
- Pick the prices strategy you want and type in the required information and facts. Make your accounts and purchase the transaction using your PayPal accounts or bank card.
- Opt for the submit format and acquire the authorized document format to the device.
- Complete, revise and print and sign the attained Tennessee Notice of Special Enrollment Rights.
US Legal Forms is the largest library of authorized varieties for which you can find numerous document templates. Make use of the company to acquire skillfully-created paperwork that stick to status demands.