Texas Notification is a state regulation that requires insurance companies and health maintenance organizations (HMO's) to inform Texan consumers that they are acting as an administrator for a health plan or insurance policy. The notification includes a brief description of the plan or policy, a list of the services that are covered, and information about how to file a claim. It also includes information about how to contact the insurer or HMO if the consumer has any questions or complaints. There are two types of Texas Notification: 1. Texas Notification to Insureds: This notification must be provided to insureds who are part of an insurance plan or policy that the insurer or HMO administers. It must include a brief description of the plan or policy, a list of the services that are covered, and information about how to file a claim. 2. Texas Notification to Self-Funded Plans: This notification must be provided to individuals who are part of a self-funded plan that the insurer or HMO administers. It must include a brief description of the plan or policy, a list of the services that are covered, and information about how to file a claim. Additionally, it must include information about the applicable state and federal laws that apply to self-funded plans.
Texas Notification that an Insurer or HMO will be acting as an Administrator
Description
Get your form ready online
Our built-in tools help you complete, sign, share, and store your documents in one place.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Looking for another form?
How to fill out Texas Notification That An Insurer Or HMO Will Be Acting As An Administrator?
Coping with official documentation requires attention, precision, and using well-drafted templates. US Legal Forms has been helping people across the country do just that for 25 years, so when you pick your Texas Notification that an Insurer or HMO will be acting as an Administrator template from our service, you can be sure it meets federal and state regulations.
Working with our service is simple and fast. To obtain the necessary paperwork, all you’ll need is an account with a valid subscription. Here’s a brief guideline for you to obtain your Texas Notification that an Insurer or HMO will be acting as an Administrator within minutes:
- Remember to carefully look through the form content and its correspondence with general and law requirements by previewing it or reading its description.
- Look for an alternative formal template if the previously opened one doesn’t suit your situation or state regulations (the tab for that is on the top page corner).
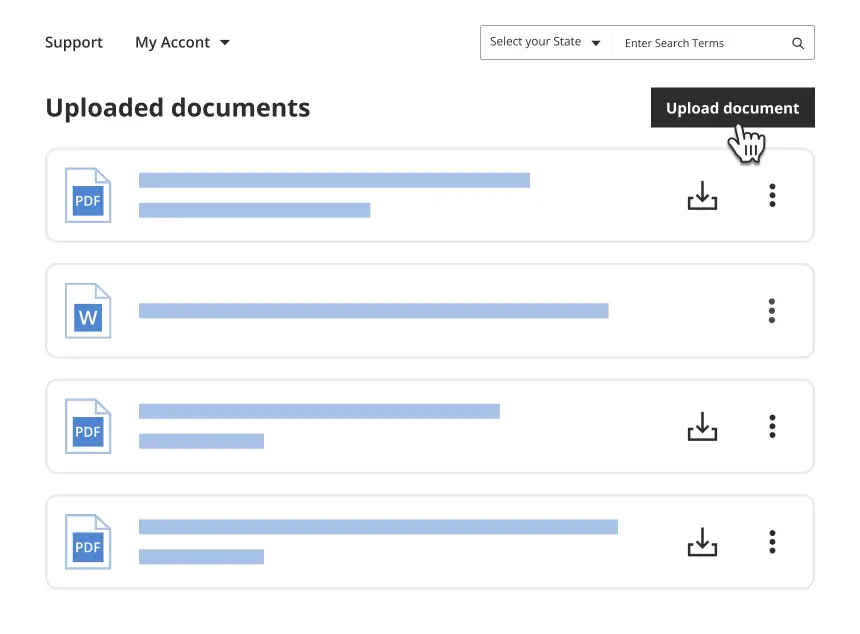
- Log in to your account and download the Texas Notification that an Insurer or HMO will be acting as an Administrator in the format you prefer. If it’s your first experience with our website, click Buy now to proceed.
- Create an account, decide on your subscription plan, and pay with your credit card or PayPal account.
- Choose in what format you want to obtain your form and click Download. Print the blank or add it to a professional PDF editor to prepare it paper-free.
All documents are created for multi-usage, like the Texas Notification that an Insurer or HMO will be acting as an Administrator you see on this page. If you need them in the future, you can fill them out without re-payment - just open the My Forms tab in your profile and complete your document whenever you need it. Try US Legal Forms and prepare your business and personal paperwork rapidly and in full legal compliance!
Form popularity
FAQ
Onset of symptoms less than three hours before beginning treatment. No head trauma or prior stroke in the past three months. No heart attack (myocardial infarction) in the past three months. No gastrointestinal or genitourinary hemorrhage in the past 21 days.
TPA stands for Third Party Administrator and as such is defined as an organization or individual that handles the claims, processing, and reporting components of a self-funded health benefits plan.
party administrator is an organization that conducts the administrative and operational work for an insurance plan. The administrative work often includes processing claims, enrolling customers, collecting premiums, and complying with federal regulations.
Third Party Administrators (TPA)
? Patients who have a persistent neurologic deficit that is potentially disabling, despite improvement of any degree, should be treated with tPA in the absence of other contraindications. Any of the following should be considered disabling deficits: Complete hemianopia: ?2 on NIHSS question 3, or.
Other Contraindications for tPA Significant head trauma or prior stroke in the previous 3 months. Symptoms suggest subarachnoid hemorrhage. Arterial puncture at a noncompressible site in the previous 7 days.
A TPA shall maintain minimum paid up equity share capital of not less than rupees four crores. The net worth of a TPA shall at no time during the period of registration fall below rupees one crore.
Because tPA increases the risk of bleeding, patients who have a history of bleeding problems, recent surgery or trauma, uncontrolled high blood pressure or recent head injury may not be able to receive it.