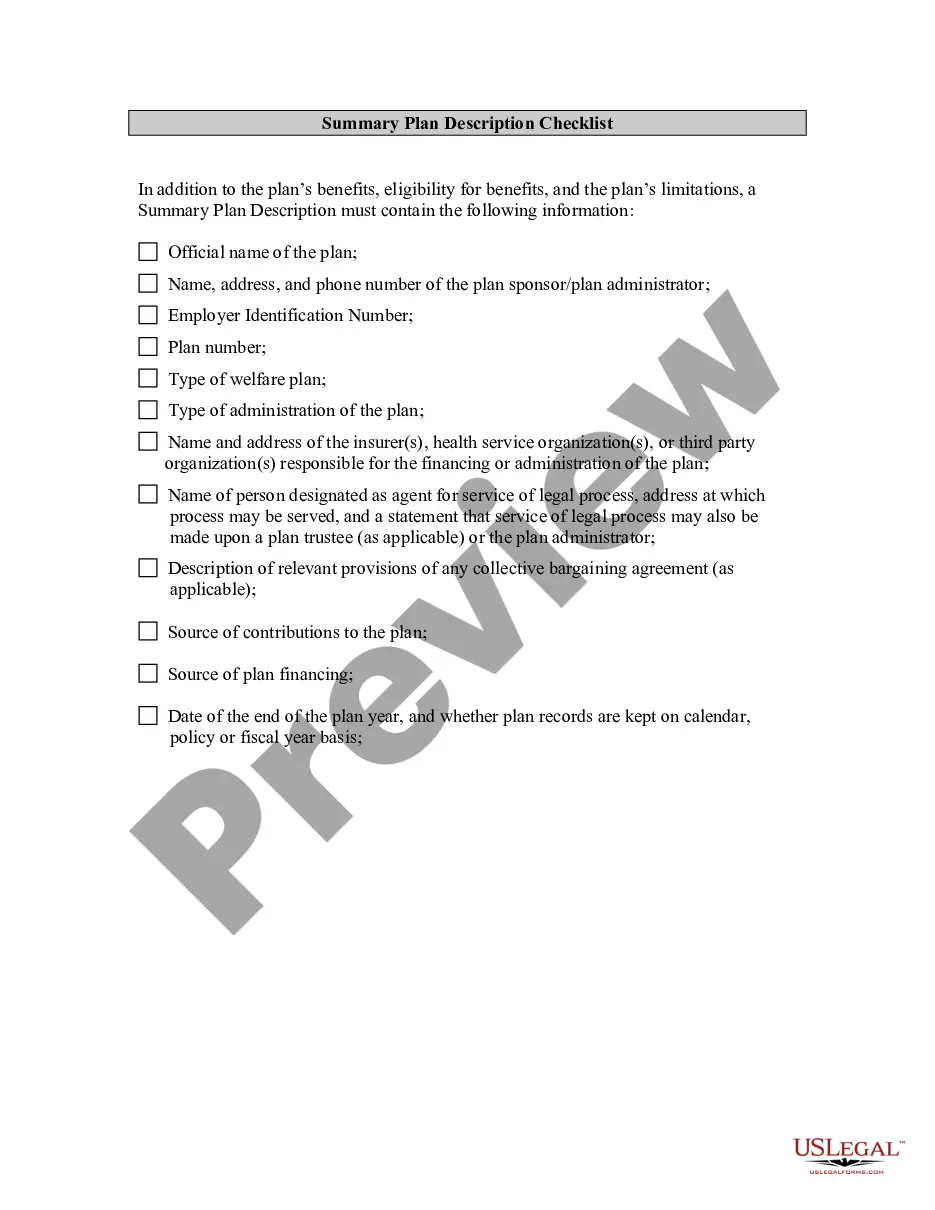
The Texas Consumer Choice Evidence of Coverage (EOC) Checklist — Large Employer and Conversion Plans is a document used by employers in Texas to provide clear information about their health insurance plans. It includes key information such as plan benefits and costs, deductibles, coinsurance, out-of-pocket maximums, networks, and other important details. It also includes a checklist of items that employers must review to ensure compliance with Texas regulations. The checklist is divided into two categories: Large Employer Plans and Conversion Plans. Large Employer Plans include those that are subject to the requirements of the Affordable Care Act (ACA) and meet certain criteria, such as having at least 50 full-time employees. Conversion Plans are those that are not subject to the ACA and are offered to groups of fewer than 50 employees. The Texas Consumer Choice Evidence of Coverage (EOC) Checklist — Large Employer and Conversion Plans includes the following items: — Plan Summary: A summary of the plan's benefits, deductibles, coinsurance, out-of-pocket maximums, and other details. — Network of Providers: A list of in-network providers and the type of care they provide. — Cost-Sharing Requirements: Information about deductibles, coinsurance, co-payments, and out-of-pocket maximums. — Coverage Limitations: Details about any limitations or exclusions on coverage. — Claims Procedures: Information about the process for filing claims and receiving reimbursement. — Grievance Procedures: A description of how to file a complaint about a plan or provider. — Texas Consumer Choice Evidence of Coverage (EOC): A document that outlines the plan's benefits, costs, and other relevant information in accordance with Texas regulations. — Large Employer and Conversion Plan Checklist: A checklist that employers use to ensure compliance with Texas regulations.
Texas Consumer Choice Evidence of Coverage (EOC) Checklist - Large Employer and Conversion Plans
Description
How to fill out Texas Consumer Choice Evidence Of Coverage (EOC) Checklist - Large Employer And Conversion Plans?
If you’re searching for a way to appropriately complete the Texas Consumer Choice Evidence of Coverage (EOC) Checklist - Large Employer and Conversion Plans without hiring a legal representative, then you’re just in the right place. US Legal Forms has proven itself as the most extensive and reliable library of official templates for every personal and business situation. Every piece of documentation you find on our online service is created in accordance with nationwide and state laws, so you can be certain that your documents are in order.
Adhere to these simple guidelines on how to obtain the ready-to-use Texas Consumer Choice Evidence of Coverage (EOC) Checklist - Large Employer and Conversion Plans:
- Ensure the document you see on the page corresponds with your legal situation and state laws by examining its text description or looking through the Preview mode.
- Enter the document title in the Search tab on the top of the page and choose your state from the list to locate another template in case of any inconsistencies.
- Repeat with the content verification and click Buy now when you are confident with the paperwork compliance with all the demands.
- Log in to your account and click Download. Register for the service and opt for the subscription plan if you still don’t have one.
- Use your credit card or the PayPal option to purchase your US Legal Forms subscription. The document will be available to download right after.
- Choose in what format you want to get your Texas Consumer Choice Evidence of Coverage (EOC) Checklist - Large Employer and Conversion Plans and download it by clicking the appropriate button.
- Add your template to an online editor to fill out and sign it rapidly or print it out to prepare your paper copy manually.
Another great thing about US Legal Forms is that you never lose the paperwork you purchased - you can pick any of your downloaded blanks in the My Forms tab of your profile whenever you need it.