Texas Request for Review by an IRO
Description
How to fill out Texas Request For Review By An IRO?
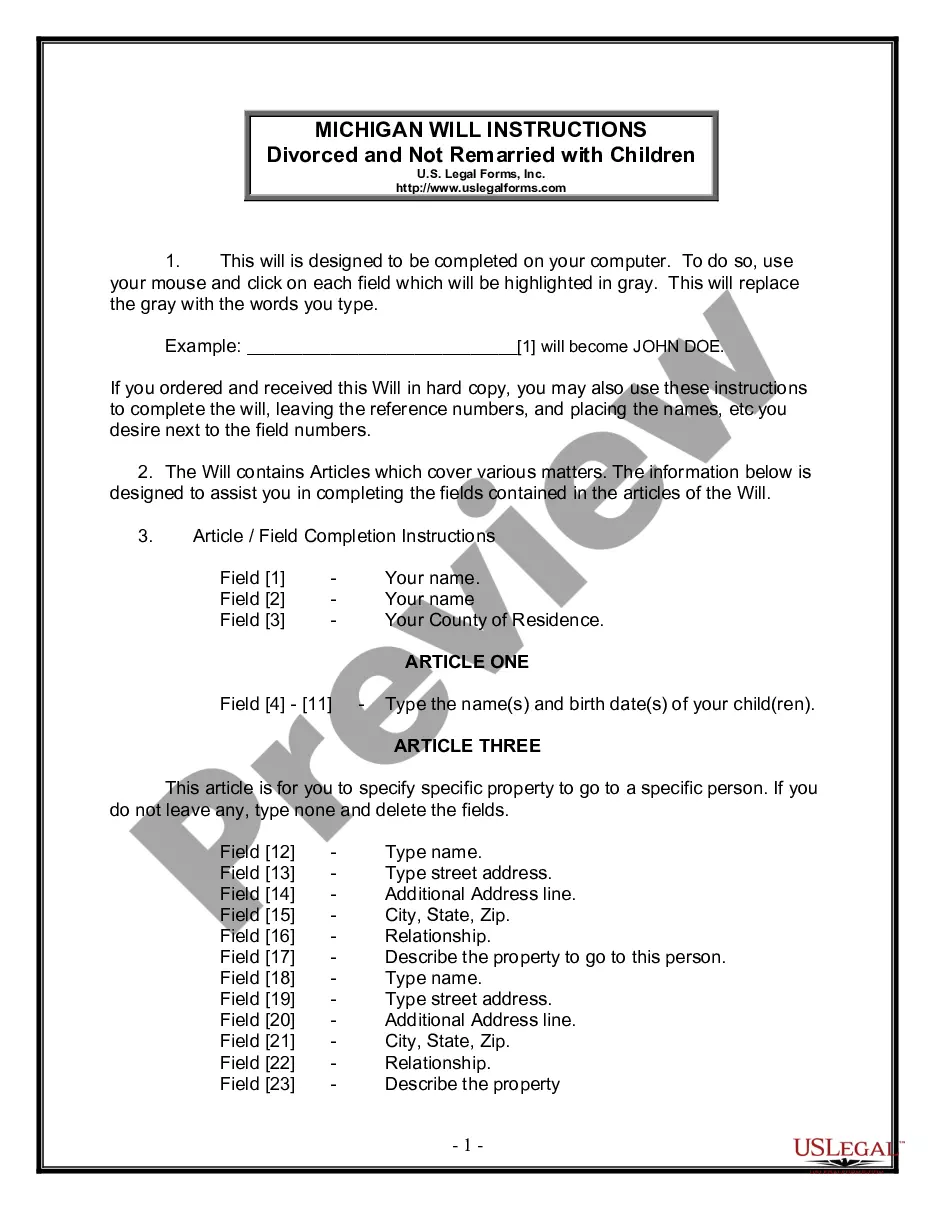
Dealing with legal documentation requires attention, precision, and using well-drafted templates. US Legal Forms has been helping people countrywide do just that for 25 years, so when you pick your Texas Request for Review by an IRO template from our library, you can be certain it meets federal and state laws.
Dealing with our service is simple and fast. To obtain the required paperwork, all you’ll need is an account with a valid subscription. Here’s a brief guideline for you to obtain your Texas Request for Review by an IRO within minutes:
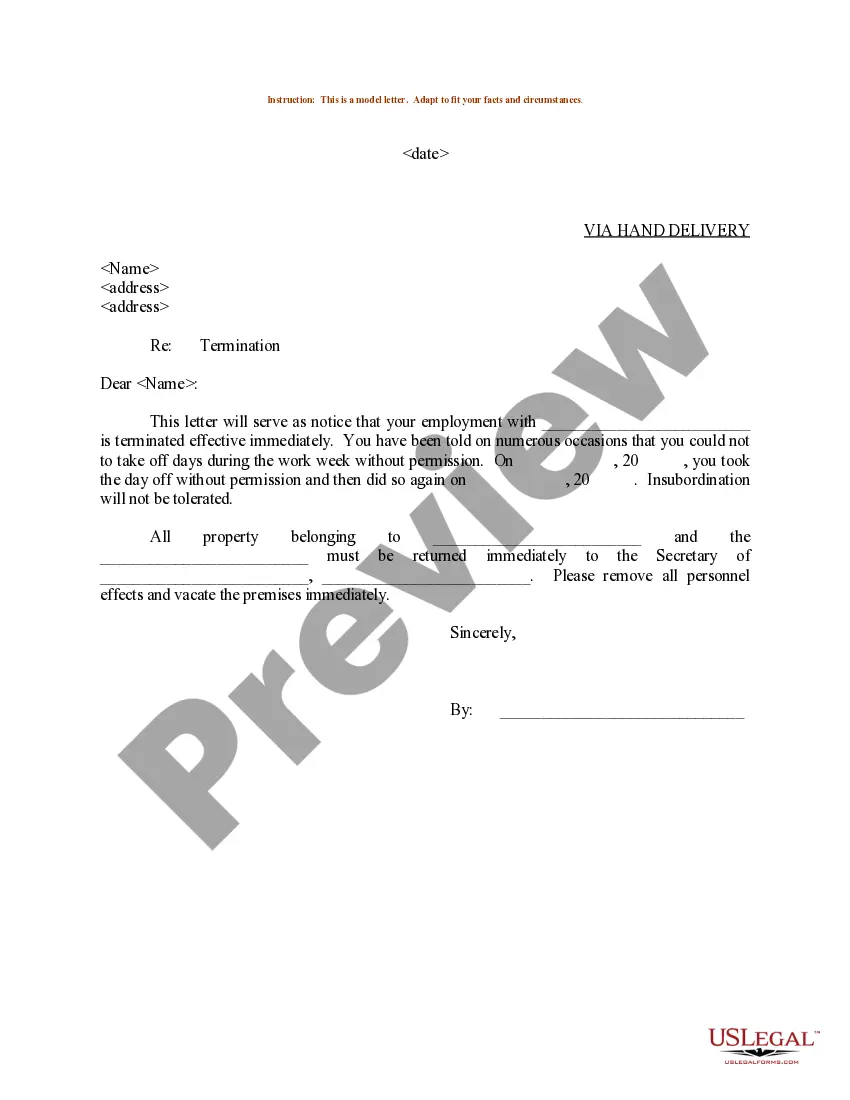
- Remember to attentively check the form content and its correspondence with general and law requirements by previewing it or reading its description.
- Look for an alternative official blank if the previously opened one doesn’t suit your situation or state regulations (the tab for that is on the top page corner).
- Log in to your account and save the Texas Request for Review by an IRO in the format you need. If it’s your first time with our service, click Buy now to proceed.
- Create an account, select your subscription plan, and pay with your credit card or PayPal account.
- Choose in what format you want to obtain your form and click Download. Print the blank or add it to a professional PDF editor to submit it electronically.
All documents are drafted for multi-usage, like the Texas Request for Review by an IRO you see on this page. If you need them in the future, you can fill them out without re-payment - just open the My Forms tab in your profile and complete your document whenever you need it. Try US Legal Forms and prepare your business and personal paperwork quickly and in full legal compliance!
Form popularity
FAQ
What is an independent review organization (IRO)? If your health plan upholds a claim denial after you completed its appeals process, you can request an external review of your appeal using an independent review organization (IRO).
An Independent Review Organization (IRO) provides independent medical reviews to help insurance payers make consistent, evidence-based healthcare decisions in regards to benefits coverage.
An IRO determines the medical necessity and appropriateness of health care delivered or proposed to be delivered by a health care provider.
Under the Affordable Care Act (ACA) and at the request of a plan participant or beneficiary, a group health plan or health insurer must assign an impartial third party, known as an independent review organization (IRO), to perform external review of a final benefits denial under the plan's internal administrative
A: Independent Review Organization (IRO) fees are divided into two tiers. Tier 1 is a review performed by a doctor of medicine or a doctor of osteopathy. The fee for a Tier 1 review is $650.00. Tier 2 includes all other types of health care providers.
An Independent Review Organization (IRO) provides independent medical reviews to help insurance payers make consistent, evidence-based healthcare decisions in regards to benefits coverage.
A reliable IRO uses physician matching, which ensures reviews are managed with the highest level of knowledge and expertise using widely accepted criteria, and offers immediate access to physicians and allied health care practitioners who are leaders in medical treatments and services.
WHAT IS AN IRO? Within the health care industry, an independent review organization (IRO) acts as a third-party medical review resource which provides objective, unbiased medical determinations that support effective decision making, based only on medical evidence.