Texas Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
Choosing the right authorized document web template can be quite a battle. Obviously, there are a lot of layouts available online, but how do you get the authorized type you need? Take advantage of the US Legal Forms website. The services delivers a large number of layouts, for example the Texas Sample COBRA Enrollment and / or Waiver Letter, which you can use for business and personal demands. All of the kinds are checked by pros and fulfill federal and state specifications.
If you are presently listed, log in to the accounts and click on the Acquire switch to have the Texas Sample COBRA Enrollment and / or Waiver Letter. Make use of accounts to check throughout the authorized kinds you may have ordered formerly. Check out the My Forms tab of your own accounts and have an additional version from the document you need.
If you are a new user of US Legal Forms, allow me to share basic directions so that you can follow:
- Initially, make sure you have selected the appropriate type for your town/state. You can look through the form utilizing the Preview switch and look at the form information to ensure this is basically the right one for you.
- If the type does not fulfill your requirements, make use of the Seach area to get the right type.
- When you are certain that the form is acceptable, click on the Acquire now switch to have the type.
- Pick the pricing program you would like and type in the necessary information. Create your accounts and purchase an order using your PayPal accounts or credit card.
- Select the document structure and obtain the authorized document web template to the product.
- Complete, modify and produce and sign the obtained Texas Sample COBRA Enrollment and / or Waiver Letter.
US Legal Forms is the greatest library of authorized kinds where you can see numerous document layouts. Take advantage of the company to obtain expertly-made files that follow express specifications.
Form popularity
FAQ
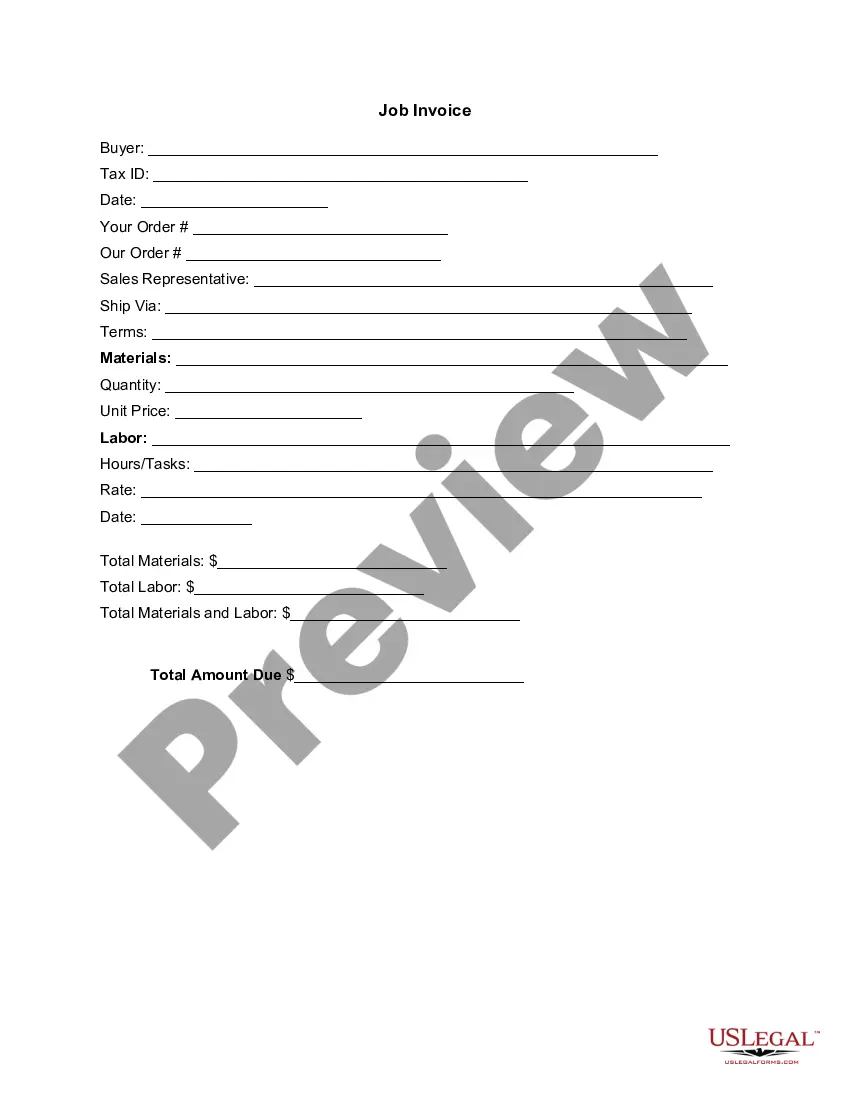
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
A COBRA letter is drafted by the plan administrator with a copy mailed to each qualified beneficiary before the coverage is terminated. The COBRA termination letter format must include the reason why the coverageis being terminated, the rights of the beneficiaries, and the specific date the coverage will end.
STATE CONTINUATION: If you are not eligible for COBRA or if you have exhausted your COBRA coverage, Texas law provides you with coverage continuation rights.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
For groups subject to COBRA, Texas law allows an additional six (6) months of coverage after COBRA ends. The law applies only to fully insured groups. COBRA participants are eligible for the additional six (6) months of continuation coverage after 18, 29, or 36 months of COBRA coverage.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Under Texas state continuation, you and your family may remain covered under your former employer's health plan for up to nine months if you are not eligible for COBRA.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.