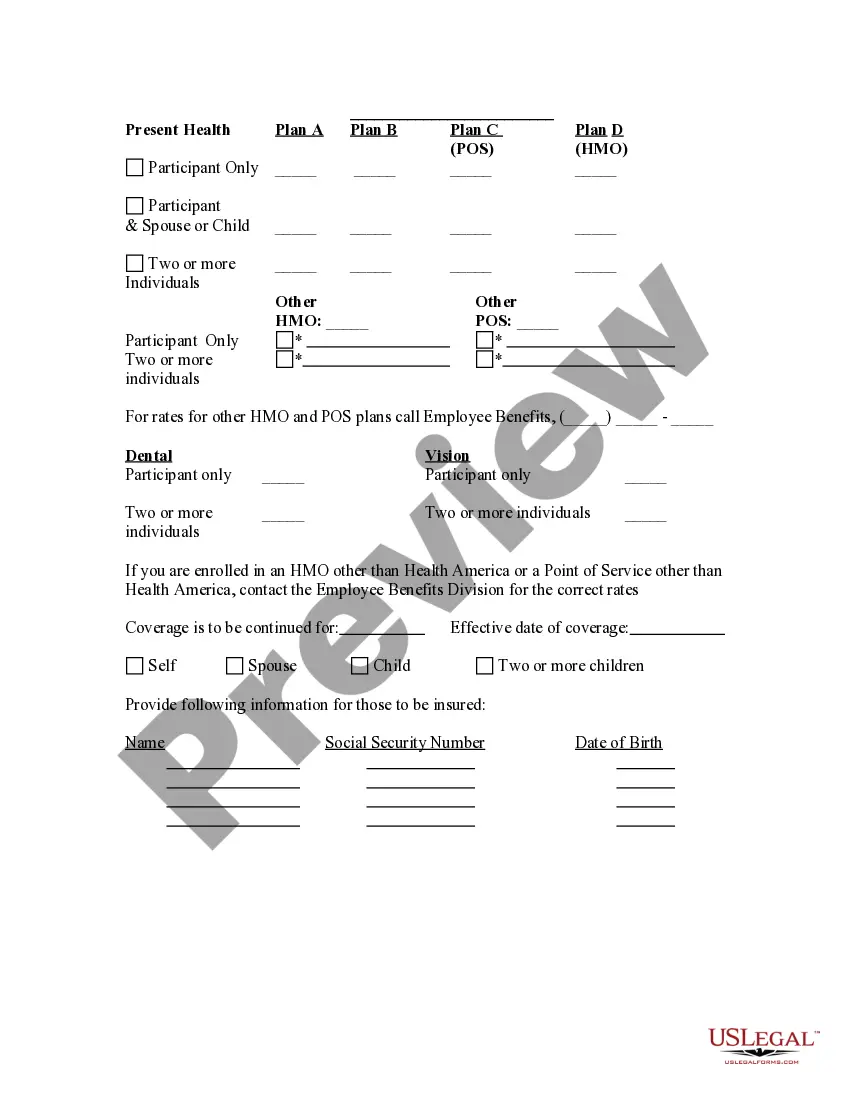
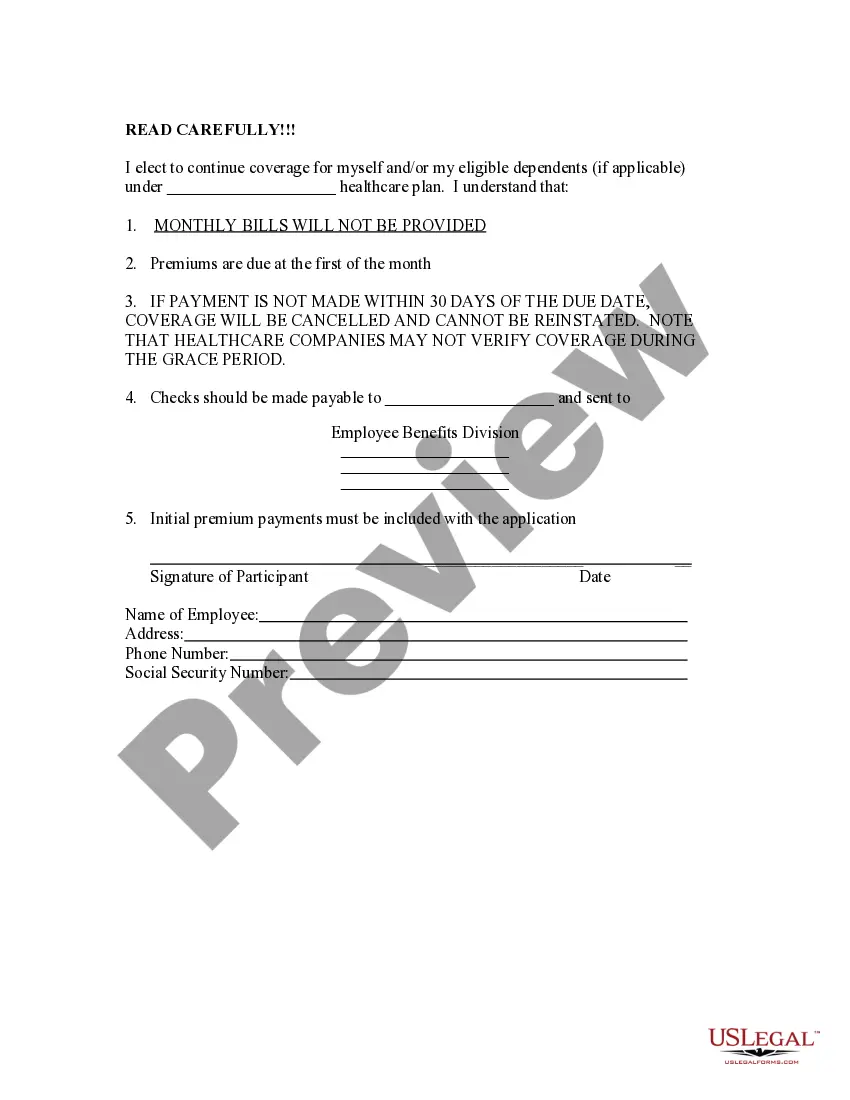
The Texas Election Form for Continuation of Benefits, also known as COBRA, is an essential document that provides individuals with the option to extend their health benefits coverage after experiencing job loss or other qualifying events. COBRA stands for Consolidated Omnibus Budget Reconciliation Act, a federal law that ensures employees and their families have the opportunity to continue their group health insurance coverage for a limited period. There are different types of Texas Election Forms for Continuation of Benefits — COBRA that individuals may encounter, depending on their specific circumstances. The most common COBRA forms include: 1. Texas Election Form for COBRA — Initial Qualifying Event: This form is used when an eligible individual experiences a qualifying event, such as job termination, reduction in work hours, or the death of an employee if coverage was provided through the employment-based plan. It allows the employee or their covered dependents to elect continued health coverage by submitting the form to the plan administrator within the specified timeframe. 2. Texas Election Form for COBRA — Extended Qualifying Event: This form is utilized when there is an extension of the maximum coverage period due to a second qualifying event. For instance, if a covered employee divorced, resulting in the loss of coverage, the dependent spouse and children may be eligible for an extended COBRA coverage period. The extended qualifying event form must be completed to request an extension of coverage. 3. Texas Election Form for COBRA — Open Enrollment: This form comes into play during the annual open enrollment periods. It allows individuals to enroll or re-enroll in COBRA coverage, even if they had previously declined it or were not eligible. 4. Texas Election Form for COBRA — Disability Extension: If a qualified beneficiary experiences a disability during the initial COBRA coverage period, they may be entitled to an extension of coverage. The disability extension form should be submitted, along with the required documentation, to request the continuation of benefits. It is important to note that these forms may have different names or variations depending on the specific health insurance plan being offered. The employer or health plan administrator should provide the necessary COBRA election forms and information to eligible individuals to ensure a seamless continuation of benefits process.
Texas Election Form for Continuation of Benefits - COBRA
Description
How to fill out Texas Election Form For Continuation Of Benefits - COBRA?
You may commit several hours on-line attempting to find the lawful papers format that meets the state and federal specifications you want. US Legal Forms offers a huge number of lawful forms that are evaluated by pros. You can actually download or produce the Texas Election Form for Continuation of Benefits - COBRA from our service.
If you have a US Legal Forms bank account, you are able to log in and then click the Acquire key. Afterward, you are able to total, change, produce, or sign the Texas Election Form for Continuation of Benefits - COBRA. Every lawful papers format you purchase is your own property forever. To obtain another copy of any purchased form, check out the My Forms tab and then click the corresponding key.
If you work with the US Legal Forms website the very first time, stick to the simple instructions listed below:
- First, make certain you have chosen the right papers format for the county/town of your choice. Browse the form outline to make sure you have picked the right form. If readily available, make use of the Preview key to look through the papers format too.
- In order to get another variation of your form, make use of the Research discipline to find the format that meets your requirements and specifications.
- Once you have identified the format you desire, click Get now to carry on.
- Select the pricing prepare you desire, type your qualifications, and sign up for a free account on US Legal Forms.
- Total the deal. You can utilize your bank card or PayPal bank account to pay for the lawful form.
- Select the formatting of your papers and download it to your product.
- Make changes to your papers if possible. You may total, change and sign and produce Texas Election Form for Continuation of Benefits - COBRA.
Acquire and produce a huge number of papers web templates using the US Legal Forms web site, that offers the biggest assortment of lawful forms. Use skilled and express-specific web templates to deal with your company or personal demands.