The Texas Introductory COBRA Letter is a crucial document that serves as an initial notice to individuals who are eligible for continuation of health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). COBRA guarantees employees, their spouses, and dependent children the opportunity to maintain their health insurance benefits temporarily, typically after a job loss, reduction in work hours, or other qualifying events. This introductory letter is issued by employers or their designated plan administrators in Texas, notifying eligible individuals of their rights, obligations, and options under COBRA. The content of the letter aims to inform recipients about the continuation coverage available, applicable deadlines, and the steps they should take to initiate and maintain their coverage. Keywords: Texas, introductory COBRA letter, continuation of health insurance coverage, Consolidated Omnibus Budget Reconciliation Act, COBRA, eligible individuals, employers, plan administrators, health insurance benefits, job loss, reduction in work hours, qualifying events, rights, obligations, options, recipients, coverage deadlines, initiation, maintenance. Types of Texas Introductory COBRA Letters: 1. Texas COBRA Initial Notice Letter: This type of letter is sent to eligible individuals within a specific period after a qualifying event occurs, such as termination, reduction in work hours, or end of dependent status, to inform them about their COBRA rights and options. 2. Texas COBRA Election Notice Letter: This letter is sent to eligible individuals who have been provided the initial notice, outlining the available COBRA coverage options and the deadlines for making an election. It presents details such as premium costs, coverage period, and instructions for enrollment. 3. Texas COBRA Termination Notice Letter: When an individual's COBRA coverage is terminated due to non-payment, reaching the maximum coverage period, or other reasons, this letter is sent to notify them about the end of their continuation coverage. It may suggest alternative health insurance options or inform them of any conversion rights they may have. 4. Texas COBRA Rights Extension Letter: In certain circumstances, COBRA coverage may be extended beyond the usual 18-month or 36-month period. This letter is issued to inform eligible individuals about their extended rights and the steps they need to take to maintain their coverage. Note: The actual names and formats of the letters may vary depending on the specific plan administrator or employer; however, the key information and purpose of these letters remain consistent.
Texas Introductory COBRA Letter
Description
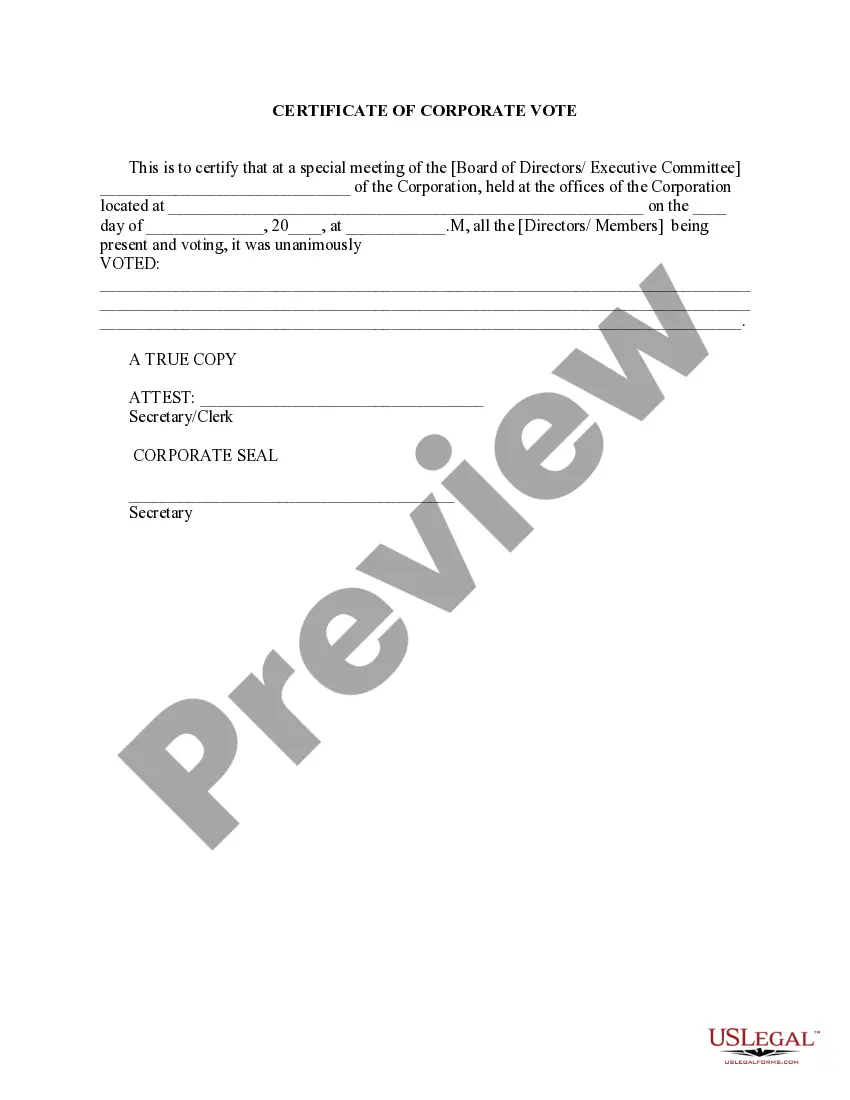
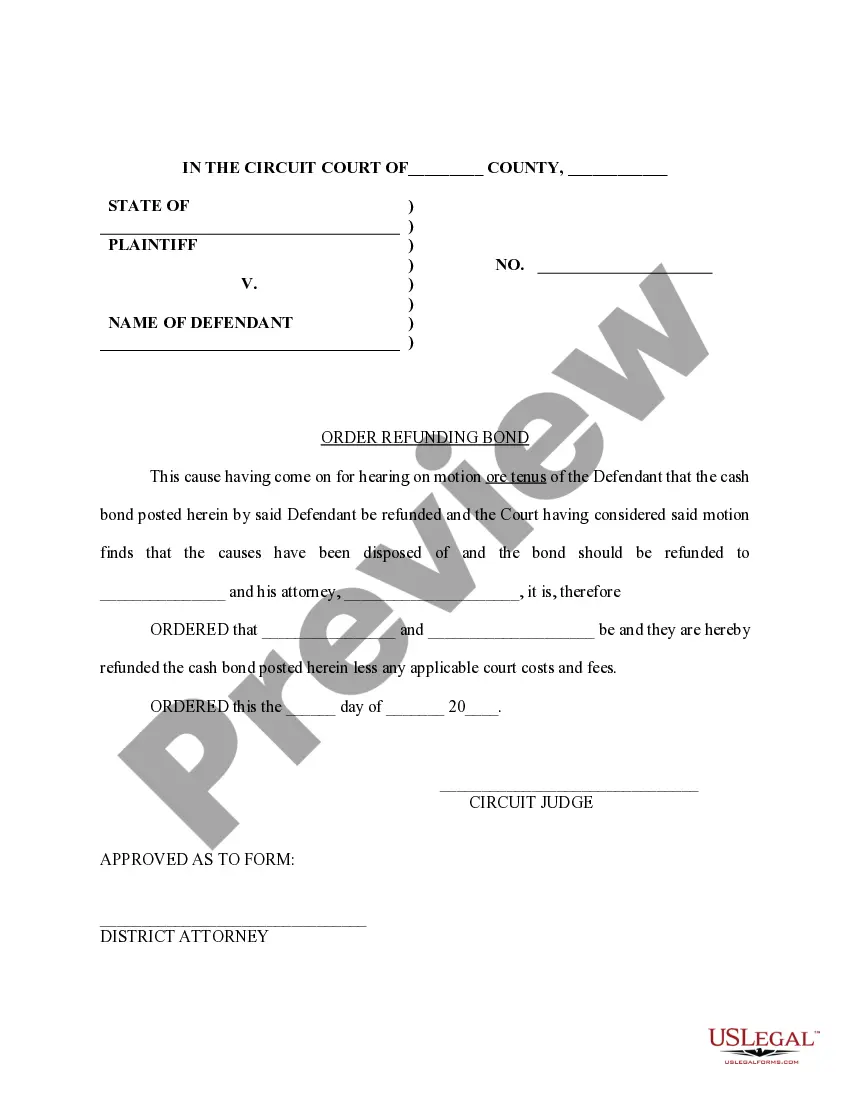
How to fill out Texas Introductory COBRA Letter?
You may invest hours on-line trying to find the lawful record format that fits the state and federal demands you require. US Legal Forms gives a large number of lawful varieties that are analyzed by specialists. It is possible to obtain or produce the Texas Introductory COBRA Letter from your support.
If you already possess a US Legal Forms accounts, you may log in and click the Download option. After that, you may complete, change, produce, or indication the Texas Introductory COBRA Letter. Each lawful record format you purchase is your own property permanently. To obtain one more copy of the purchased develop, go to the My Forms tab and click the related option.
Should you use the US Legal Forms internet site the first time, keep to the simple instructions listed below:
- First, be sure that you have selected the correct record format for that area/metropolis of your choosing. See the develop information to make sure you have chosen the appropriate develop. If offered, utilize the Review option to appear from the record format as well.
- If you wish to get one more model of the develop, utilize the Lookup industry to find the format that fits your needs and demands.
- Upon having located the format you need, just click Get now to proceed.
- Select the prices strategy you need, type in your credentials, and register for an account on US Legal Forms.
- Full the transaction. You may use your bank card or PayPal accounts to cover the lawful develop.
- Select the file format of the record and obtain it in your product.
- Make adjustments in your record if needed. You may complete, change and indication and produce Texas Introductory COBRA Letter.
Download and produce a large number of record layouts while using US Legal Forms Internet site, which offers the biggest selection of lawful varieties. Use skilled and express-certain layouts to take on your company or personal requires.