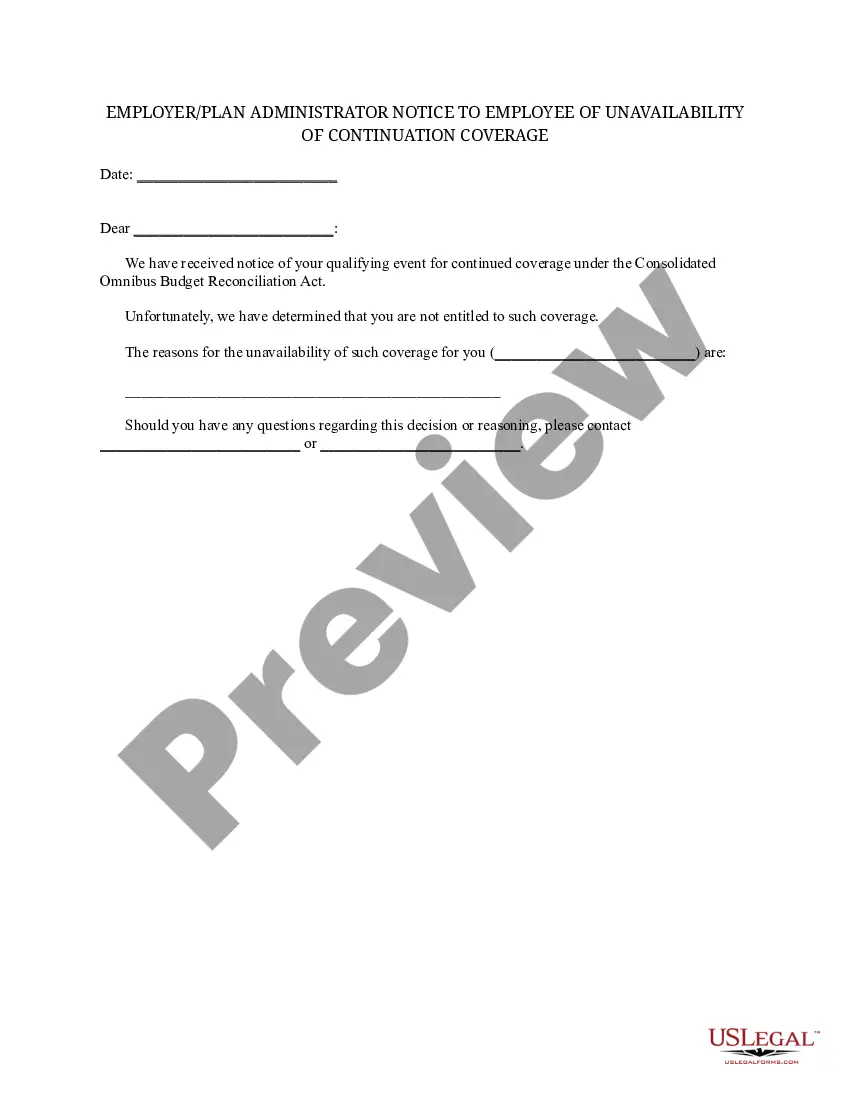
Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
US Legal Forms - one of the largest repositories of legal documents in the United States - offers a variety of legal document templates that you can download or print.
By using the website, you can obtain thousands of forms for business and personal needs, organized by categories, states, or keywords. You can find the latest versions of forms such as the Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation in a matter of seconds.
If you already hold a subscription, Log In to access Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation in the US Legal Forms library. The Download button will appear on every form you view. You can access all previously acquired forms within the My documents tab of your account.
Select the format and download the form onto your device.
Make edits. Fill out, modify, print, and sign the downloaded Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
Every template you add to your account has no expiration date and is yours permanently. Therefore, to download or print another copy, simply go to the My documents section and click on the form you require.
Access the Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation with US Legal Forms, the most extensive library of legal document templates. Utilize a multitude of professional and state-specific templates that satisfy your business or personal needs and requirements.
- If you want to use US Legal Forms for the first time, here are simple instructions to help you begin.
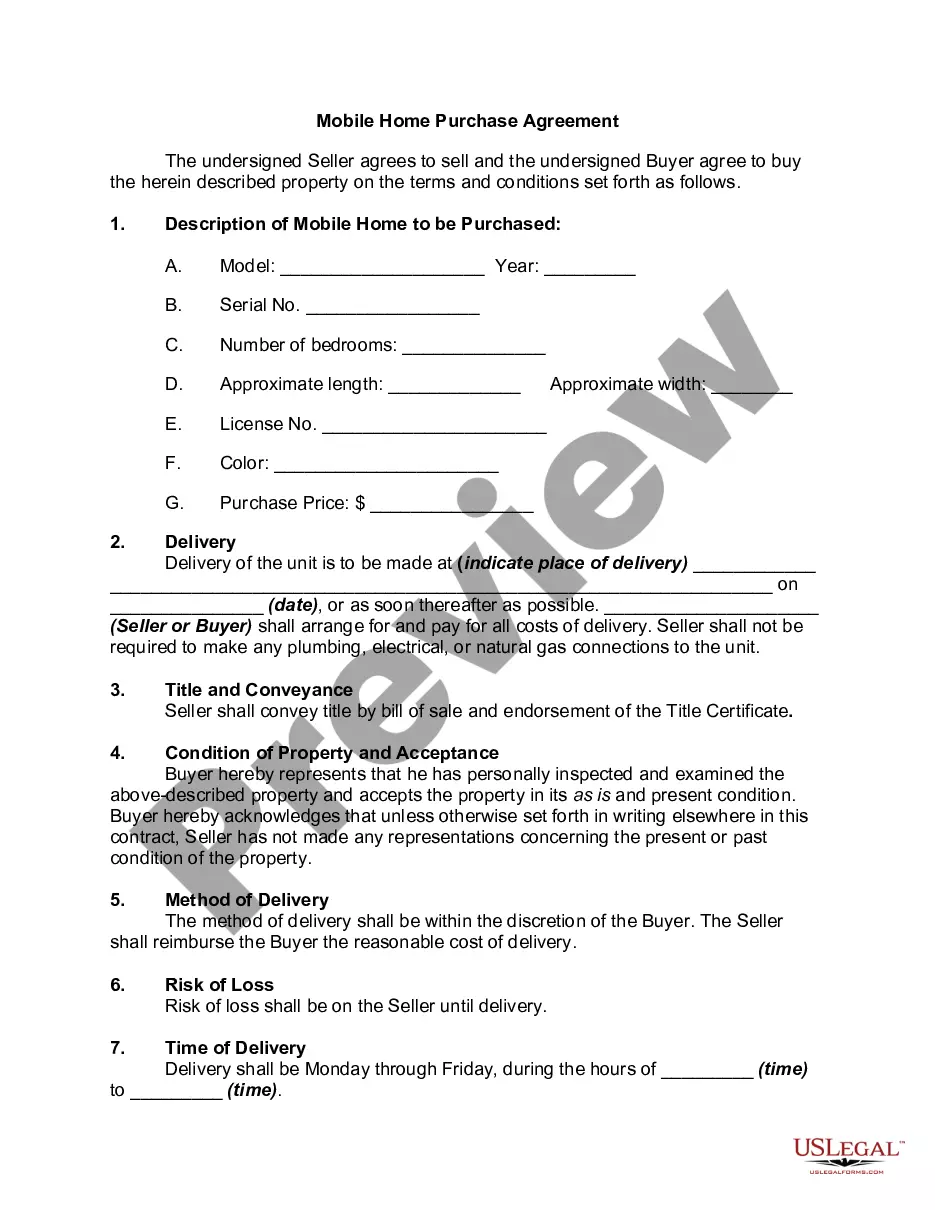
- Ensure you have selected the correct form for your city/state. Click the Preview button to review the form's content.
- Read the form description to confirm that you have chosen the correct form.
- If the form does not meet your needs, utilize the Search field at the top of the display to find the one that does.
- If you are satisfied with the form, confirm your choice by clicking the Buy now button. Then, choose the pricing plan you want and provide your details to register for an account.
- Process the transaction. Use your credit card or PayPal account to complete the transaction.
Form popularity
FAQ
While this question concerns Florida law, it's important to note that Texas follows different guidelines. In Texas, employers with less than 20 employees are generally not subject to COBRA requirements. Instead, they may be governed by Texas laws that necessitate the Texas Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
If the Qualifying Event is termination, Participating Qualified Beneficiaries have 31 days to elect and pay for the first premium from the date of termination or notification.
Under Texas state continuation, you and your family may remain covered under your former employer's health plan for up to nine months if you are not eligible for COBRA.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Cal-COBRA administration requires four basic compliance components:Notifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section.Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.More items...
Any individual who is covered under a group health plan either as the employee, the spouse of the employee, or the dependent child of the employee is eligible for the nine (9) month state continuation coverage if they have been continuously covered under the group coverage for at least three (3) consecutive months
State law allows employees of smaller employers (fewer than 20 employees) to keep the same. group health insurance coverage for up to nine months after loss of a job or loss of coverage. because of a reduction in work hours. This is called state continuation.
In most cases, COBRA provides for continuation of health plan coverage for up to 18 months following the work separation. COBRA rights accrue once a "qualifying event" occurs - basically, a qualifying event is any change in the employment relationship that results in loss of health plan benefits.
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.