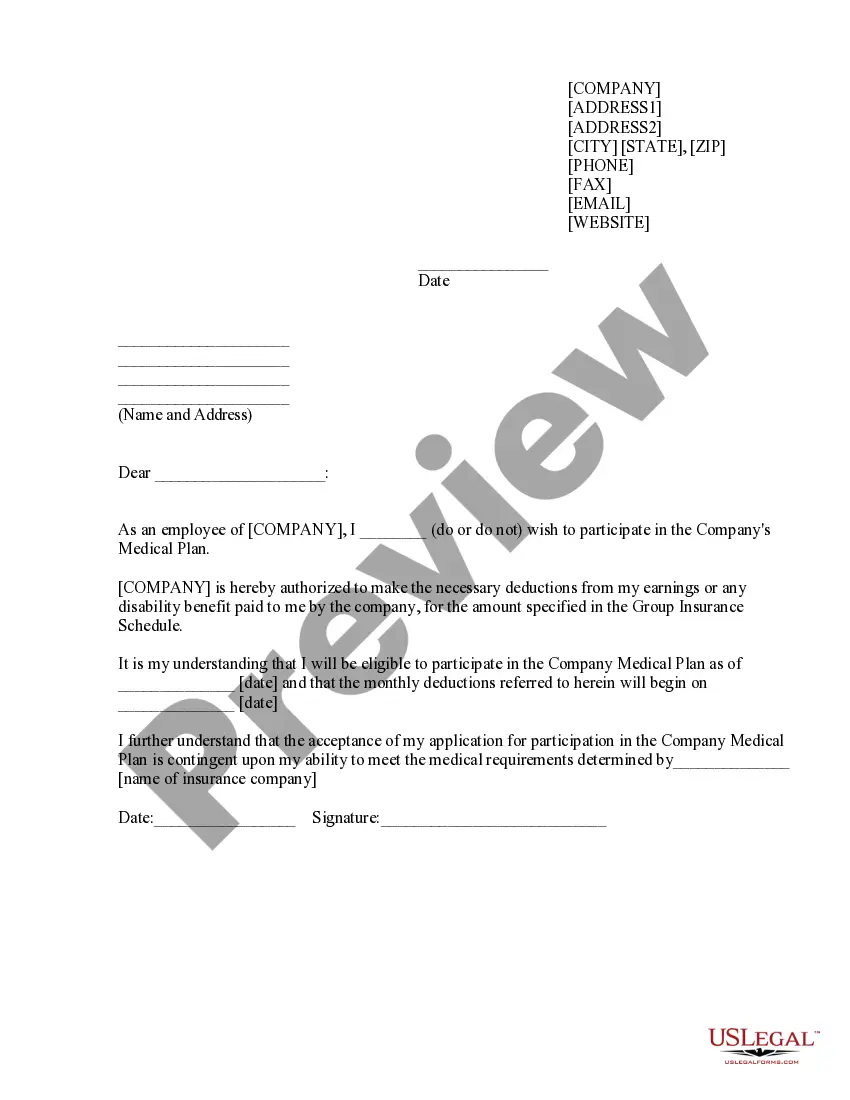
Authorization to Participate in Medical Plan is a legally binding document that allows a person to participate in a health care plan or program. It is typically used by employers who provide their employees with health insurance, as well as by individuals who purchase coverage in the individual market. The authorization contains information about the plan, including the type of coverage, the premium, co-payments and deductibles, and any other terms or conditions that may apply. It also acknowledges the participant’s agreement to abide by the terms of the plan. There are two types of Authorization to Participate in Medical Plan: active authorization and passive authorization. Active authorization requires the participant to sign the authorization form and submit it to the plan administrator for approval. Passive authorization occurs when a person is automatically enrolled in a plan, such as when an employee is automatically enrolled in an employer-sponsored health plan. In this case, the participant does not need to sign an authorization form but is instead enrolled in the plan without providing written consent.
Authorization to Participate in Medical Plan
Description
How to fill out Authorization To Participate In Medical Plan?
How much time and resources do you often spend on drafting official documentation? There’s a better way to get such forms than hiring legal experts or wasting hours searching the web for an appropriate blank. US Legal Forms is the top online library that provides professionally drafted and verified state-specific legal documents for any purpose, like the Authorization to Participate in Medical Plan.
To get and prepare an appropriate Authorization to Participate in Medical Plan blank, follow these easy steps:
- Examine the form content to make sure it meets your state requirements. To do so, read the form description or take advantage of the Preview option.
- If your legal template doesn’t meet your requirements, locate a different one using the search tab at the top of the page.
- If you are already registered with our service, log in and download the Authorization to Participate in Medical Plan. Otherwise, proceed to the next steps.
- Click Buy now once you find the correct blank. Select the subscription plan that suits you best to access our library’s full opportunities.
- Create an account and pay for your subscription. You can make a payment with your credit card or via PayPal - our service is totally reliable for that.
- Download your Authorization to Participate in Medical Plan on your device and fill it out on a printed-out hard copy or electronically.
Another benefit of our library is that you can access previously acquired documents that you securely store in your profile in the My Forms tab. Get them at any moment and re-complete your paperwork as often as you need.
Save time and effort completing legal paperwork with US Legal Forms, one of the most reliable web services. Sign up for us now!
Form popularity
FAQ
These steps are usually done manually, often through a cascade of phone calls, faxes and emails between payer and provider. The responsibility falls on the provider to continue to follow up with the insurance company until there is resolution of the prior authorization request ? an approval, redirection, or denial.
For example, services that may require pre-certification include outpatient and inpatient hospital services, observation services, invasive procedures, CT, MRI and PET scans, and colonoscopies. Patients are responsible for knowing the pre-certification requirements of their health plans.
For example, your health plan may require prior authorization for an MRI, so that they can make sure that a lower-cost x-ray wouldn't be sufficient. The service isn't being duplicated: This is a concern when multiple specialists are involved in your care.
Who is responsible for obtaining prior authorization? The healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patient's insurance provider.
authorization is a restriction placed on certain medications, tests, or health services by your insurance company that requires your doctor to first check and be granted permission before your plan will cover the item.
Prior authorization?sometimes called precertification or prior approval?is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Do I need permission or authorization from my insurance company before I get medical care? Planned admission to a hospital or skilled nursing facilities. Surgeries. Advanced imaging, such as MRIs and CT scans. Transplant and donor services. Non-emergency air ambulance transport. Medical equipment. Specialty drug treatments.
Why does my health insurance company need a prior authorization? The prior authorization process gives your health insurance company a chance to review how necessary a medical treatment or medication may be in treating your condition. For example, some brand-name medications are very costly.