COBRA Continuation Waiver Letter
Description Waiver Letter Sample
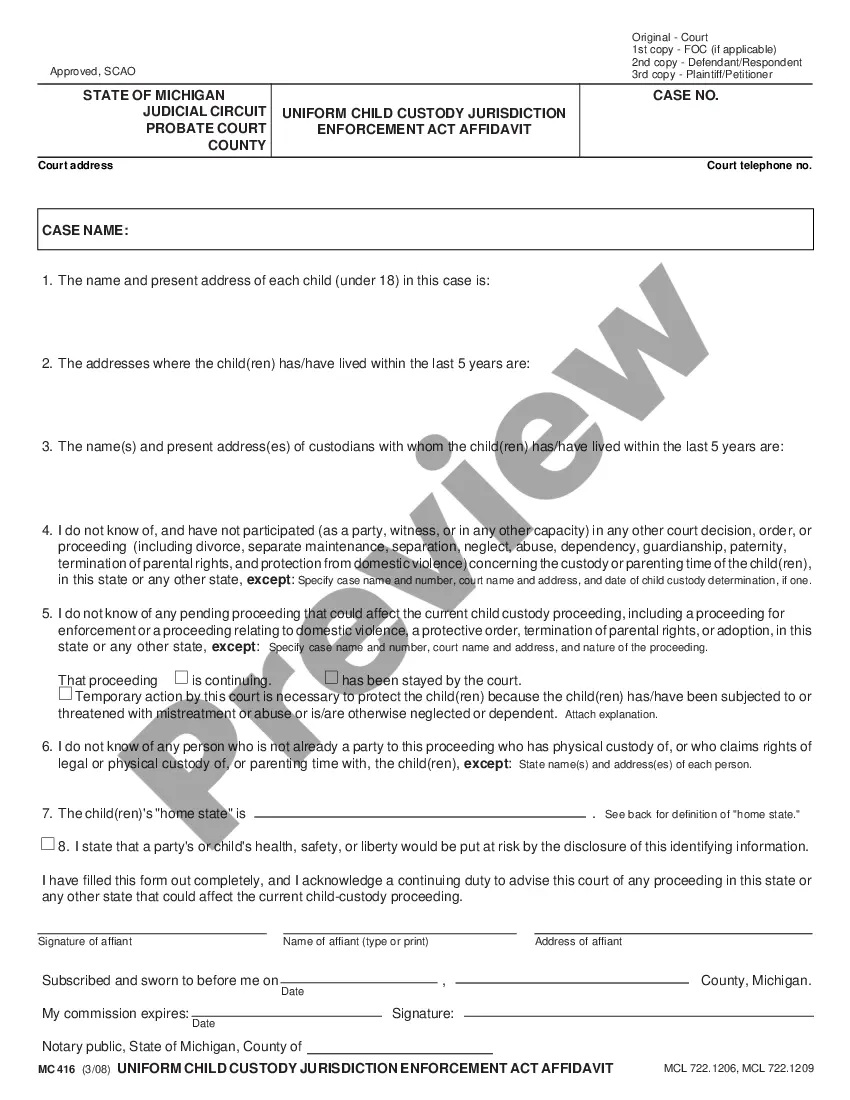
How to fill out Cobra Continuation Letter Sample?
Utilize the most extensive legal catalogue of forms. US Legal Forms is the perfect place for getting updated COBRA Continuation Waiver Letter templates. Our platform provides 1000s of legal forms drafted by certified legal professionals and categorized by state.
To download a sample from US Legal Forms, users only need to sign up for an account first. If you are already registered on our platform, log in and select the document you are looking for and purchase it. Right after purchasing forms, users can find them in the My Forms section.
To obtain a US Legal Forms subscription online, follow the guidelines listed below:
- Check if the Form name you’ve found is state-specific and suits your needs.
- In case the form features a Preview function, utilize it to review the sample.
- In case the template doesn’t suit you, utilize the search bar to find a better one.
- PressClick Buy Now if the sample corresponds to your requirements.
- Select a pricing plan.
- Create your account.
- Pay with the help of PayPal or with the credit/credit card.
- Choose a document format and download the sample.
- After it is downloaded, print it and fill it out.
Save your time and effort with the platform to find, download, and complete the Form name. Join a huge number of pleased customers who’re already using US Legal Forms!
Cobra Continuation Letter Form popularity
Cobra Letter Print Other Form Names
Continuation Letter Application FAQ
You may be eligible to apply for individual coverage through Covered California, the State's Health Benefit Exchange. You can reach Covered California at (800) 300-1506 or online at www.coveredca.com. You can apply for individual coverage directly through some health plans off the exchange.
1. You never received your COBRA enrollment packet. Contact your former employer or your health plan administrator.Your former employer must notify your health plan administrator within 30 days after your "qualifying event" death, job termination, reduced hours of employment or eligibility for Medicare.
An employer that is subject to COBRA requirements is required to notify its group health plan administrator within 30 days after an employee's employment is terminated, or employment hours are reduced.
The employer must notify the plan within 30 days of the event. You (the covered employee or one of the qualified beneficiaries) must notify the plan if the qualifying event is divorce, legal separation, or a child's loss of dependent status under the plan.
You may be eligible to apply for individual coverage through Covered California, the State's Health Benefit Exchange. You can reach Covered California at (800) 300-1506 or online at www.coveredca.com. You can apply for individual coverage directly through some health plans off the exchange.
Contact The Employer's COBRA Plan AdministratorIf your employer can not answer your questions or does not comply, you can call the Department of Labor at 1-866-487-2365.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.