Qualifying Event Notice Information for Employer to Plan Administrator
Description Information Employer Form
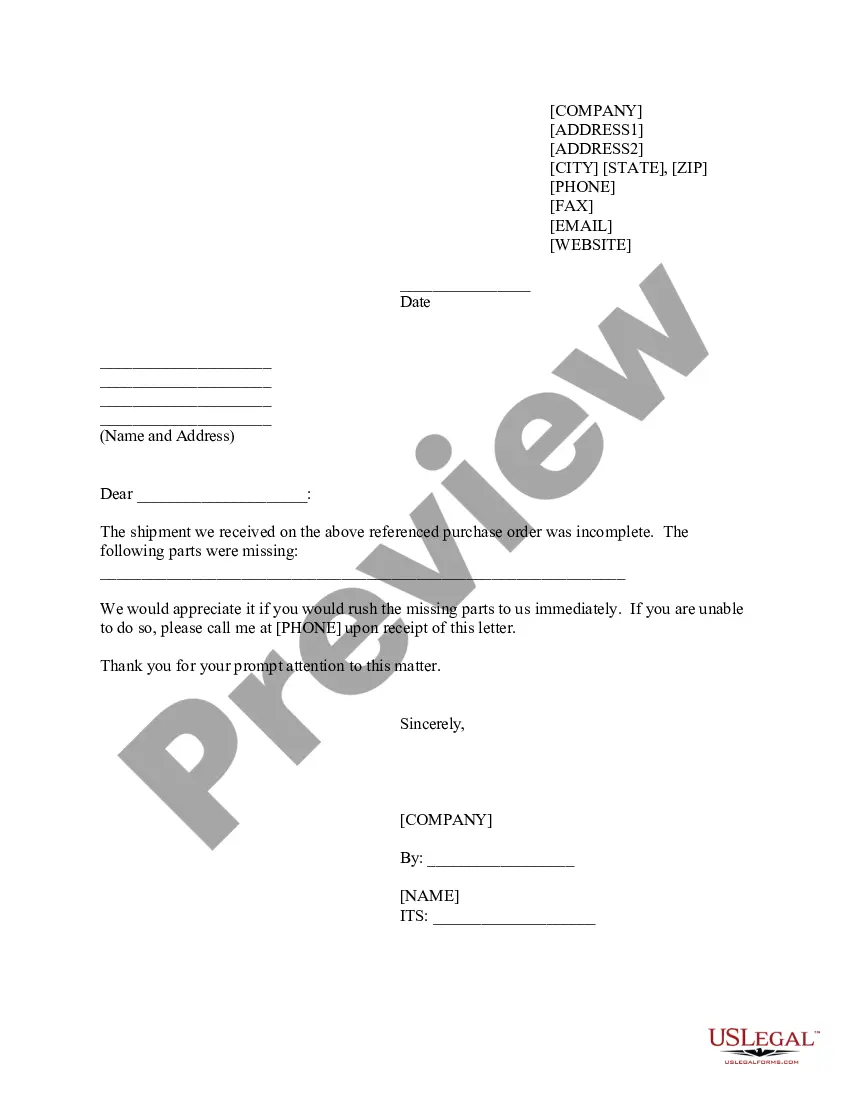
How to fill out Qualifying Employer Contract?
Use the most comprehensive legal catalogue of forms. US Legal Forms is the best place for finding up-to-date Qualifying Event Notice Information for Employer to Plan Administrator templates. Our service provides thousands of legal documents drafted by certified legal professionals and categorized by state.
To get a sample from US Legal Forms, users only need to sign up for a free account first. If you’re already registered on our platform, log in and choose the template you need and purchase it. After buying forms, users can see them in the My Forms section.
To obtain a US Legal Forms subscription online, follow the guidelines below:
- Check if the Form name you’ve found is state-specific and suits your needs.
- When the template has a Preview option, utilize it to check the sample.
- If the template does not suit you, utilize the search bar to find a better one.
- PressClick Buy Now if the template meets your expections.
- Choose a pricing plan.
- Create your account.
- Pay with the help of PayPal or with yourr debit/bank card.
- Select a document format and download the sample.
- After it’s downloaded, print it and fill it out.
Save your effort and time with the service to find, download, and fill in the Form name. Join a large number of happy clients who’re already using US Legal Forms!
Qualifying Notice Plan Form popularity
Plan Administrator Pdf Other Form Names
Qualifying Employer Pdf FAQ
Coverage is available up to $1 million per person. For more information and pricing, you can call us at 1-877-262-7241 or complete a free quote online.
Blue Shield administers Cal-COBRA when an employer is subject to it under state law. Groups have the option to self-administer their federal COBRA benefits or choose a third-party COBRA administrator, including Blue Shield's preferred COBRA administrator, CONEXIS.
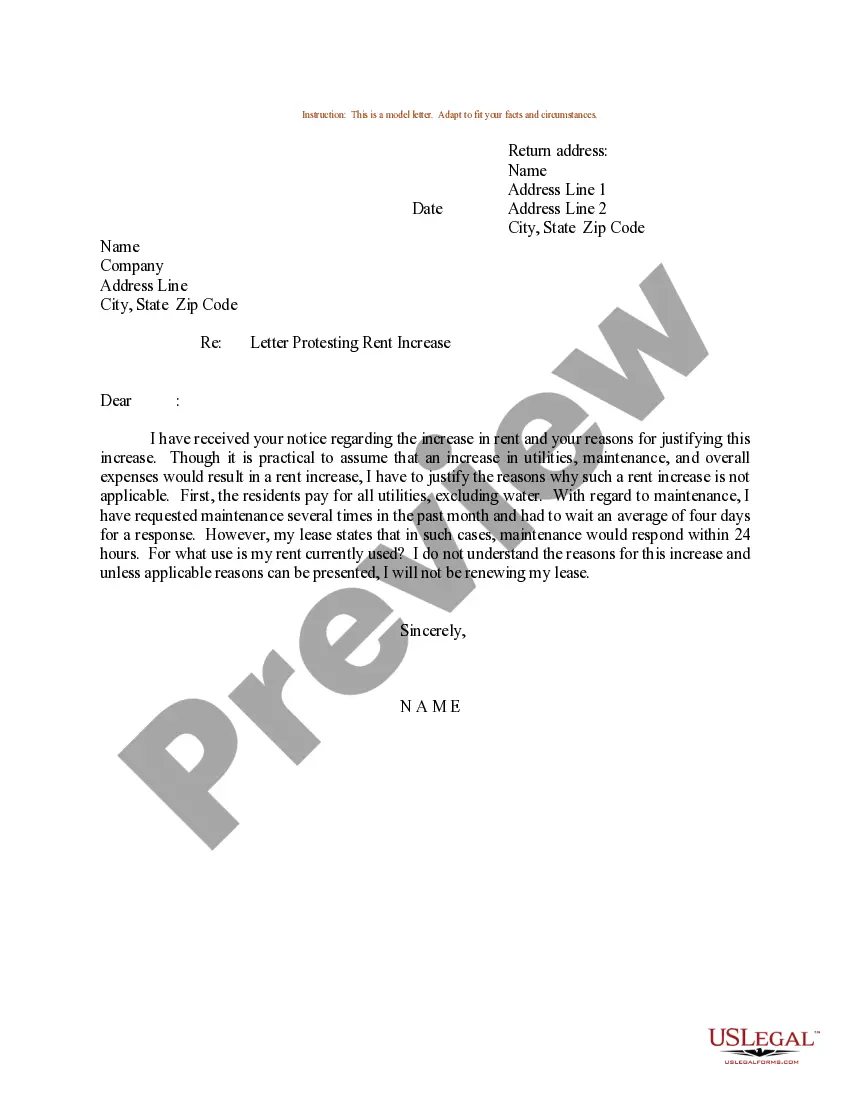
Your business has 90 days to provide the employee with a COBRA General Notice, which basically describes the employee's rights and obligations under COBRA. When a qualifying event occurs. Your business must notify the employee of their COBRA rights within 14 days of the qualifying event with an election notice.
COBRA beneficiaries pay the full health insurance premium plus a 2 percent administration fee. If monthly premiums for employees with single coverage are $200, for example; the COBRA beneficiary pays 102 percent of that amount, or $204.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
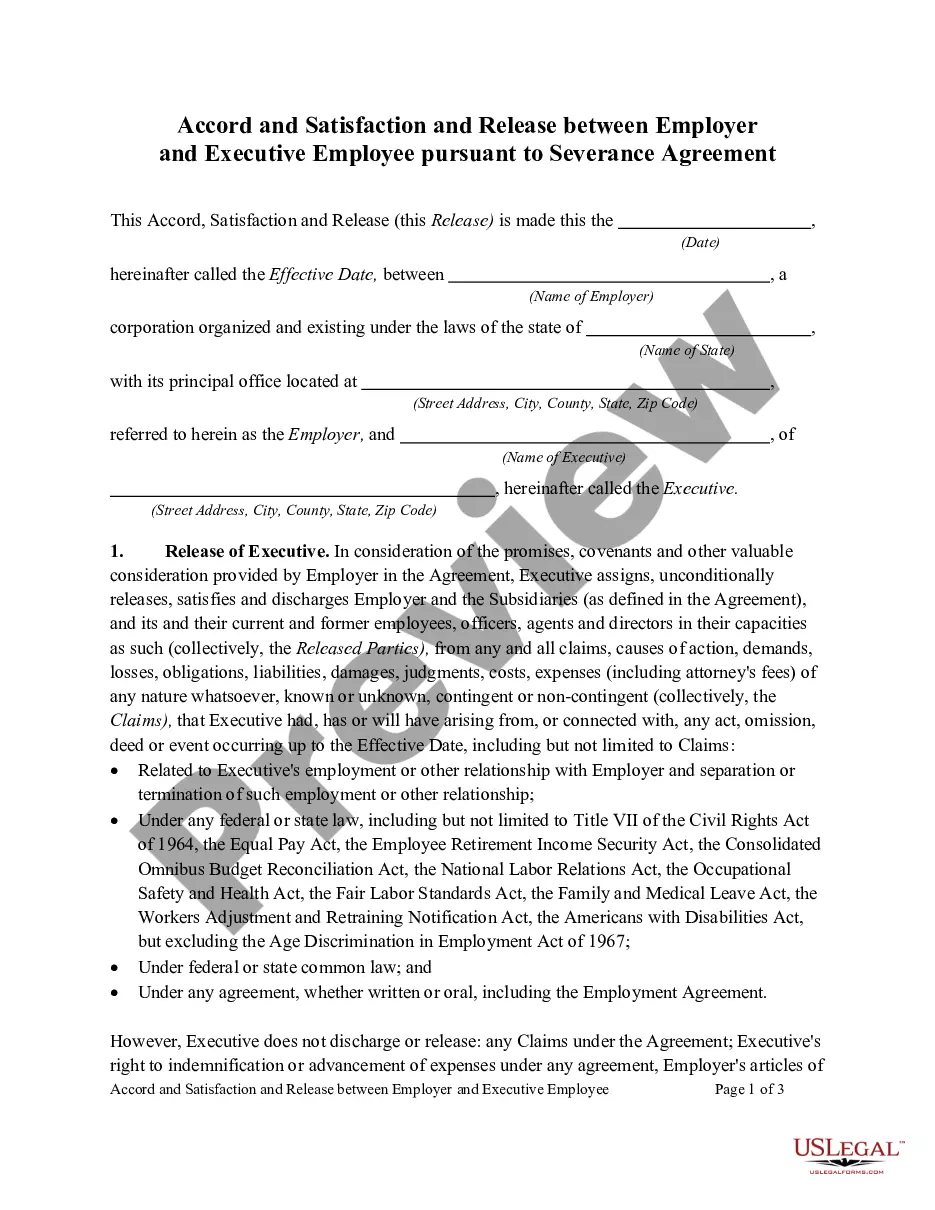
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Since losing COBRA coverage early is not a qualifying event, you would not be eligible to sign up for coverage through the Exchange. (If your COBRA runs out after the normal period, which is typically 18 or 36 months, you should be eligible for a Special Enrollment and could sign up for coverage through the Exchange).
Through the Marketplace, 1 The Department of Health and Human Services administers the COBRA provisions of the Public Health Service Act covering state and local government plans. individuals may qualify for cost-sharing reductions and a tax credit that lowers monthly premiums.
Notifying all eligible group health care participants of their COBRA rights. Providing timely notice of COBRA eligibility, enrollment forms, duration of coverage and terms of payment after a qualifying event has occurred.