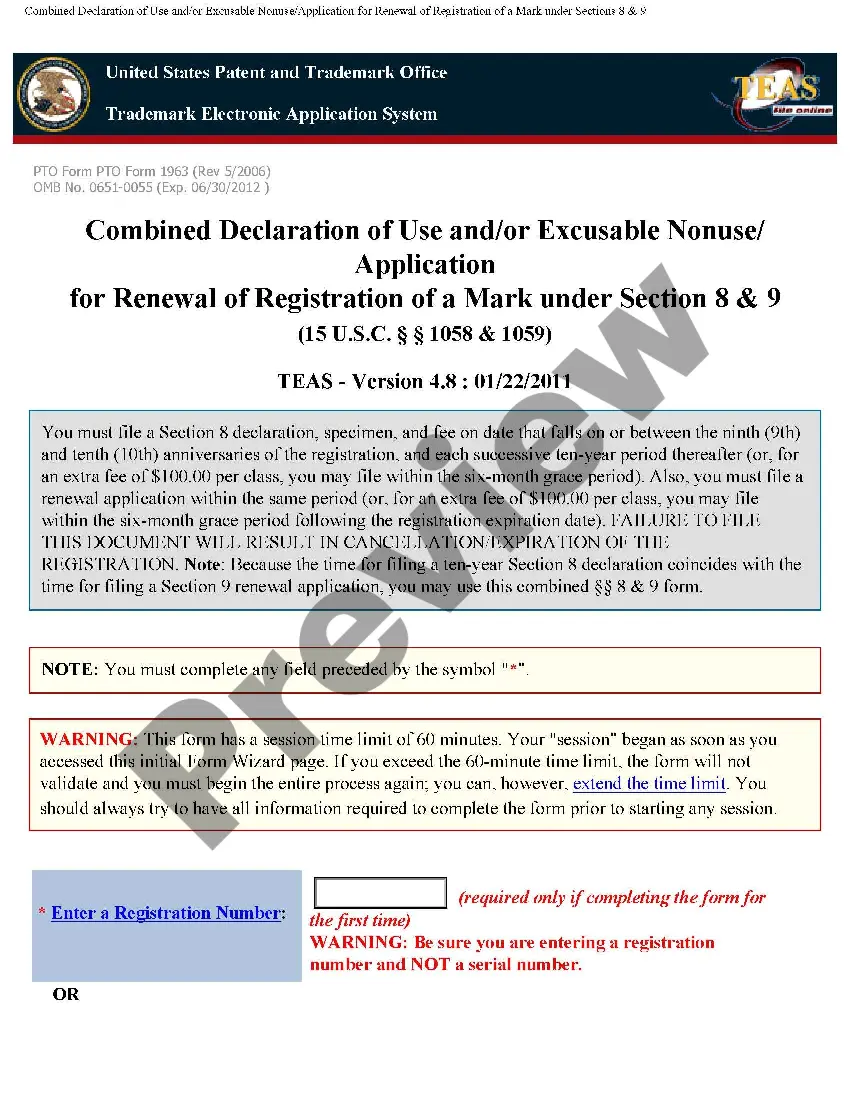
The Virginia Acknowledgment of Receipt of COBRA Notice is a crucial document that serves as proof of an individual's acknowledgment of receiving the COBRA notice, as required by federal law. COBRA (Consolidated Omnibus Budget Reconciliation Act) is a law that enables eligible employees and their beneficiaries to continue group health coverage after certain qualifying events. This acknowledgment form is specific to Virginia and must be completed by the employee or beneficiary who has received the COBRA notice. By signing this document, individuals confirm their understanding of the information provided in the notice and their awareness of the available options for continued health coverage. The Virginia Acknowledgment of Receipt of COBRA Notice contains several key elements that provide comprehensive details on the coverage continuation. It includes the effective date of the notice, the name of the employer or plan administrator, and the name of the individual receiving the notice. Additionally, the document specifies the relevant dates and deadlines for COBRA enrollment, payment procedures, and continuation period allowances. It's important to note that while there may not be different types of Virginia Acknowledgment of Receipt of COBRA Notice, it can vary in structure or presentation depending on the organization issuing it. However, the content remains consistent, emphasizing the individual's understanding of the COBRA notice and their responsibilities in accessing continued health coverage. Keywords: Virginia, Acknowledgment of Receipt, COBRA Notice, federal law, qualifying events, group health coverage, employee, beneficiary, acknowledgment form, options, continued health coverage, effective date, employer, plan administrator, dates, deadlines, enrollment, payment procedures, continuation period.
Virginia Acknowledgment of Receipt of COBRA Notice
Description
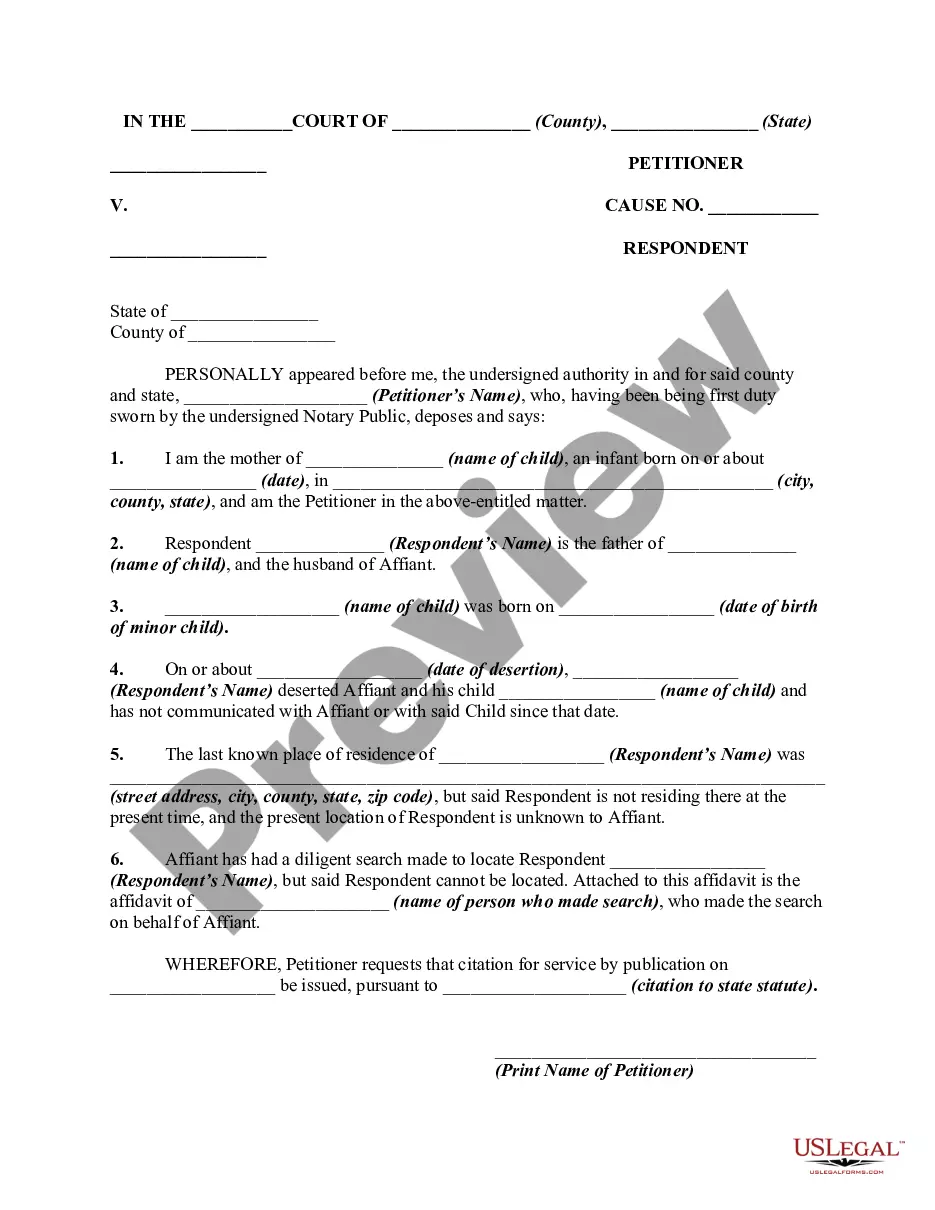
How to fill out Virginia Acknowledgment Of Receipt Of COBRA Notice?
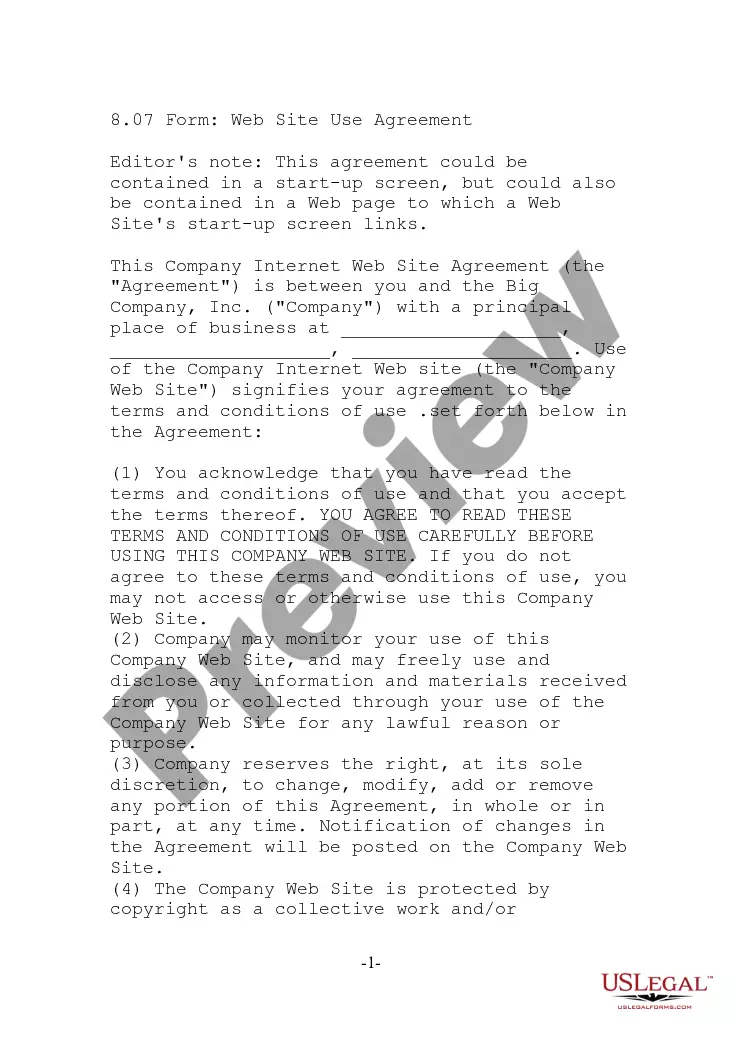
Finding the right lawful file design might be a battle. Needless to say, there are plenty of themes available on the net, but how do you obtain the lawful kind you want? Utilize the US Legal Forms internet site. The services delivers a large number of themes, for example the Virginia Acknowledgment of Receipt of COBRA Notice, that can be used for business and personal needs. All of the varieties are examined by professionals and fulfill federal and state specifications.
If you are presently listed, log in in your bank account and click on the Acquire switch to find the Virginia Acknowledgment of Receipt of COBRA Notice. Make use of bank account to search through the lawful varieties you have ordered formerly. Go to the My Forms tab of your own bank account and have an additional backup of your file you want.
If you are a fresh customer of US Legal Forms, listed here are straightforward guidelines that you can follow:
- Initially, make sure you have chosen the correct kind for your personal area/region. You may look through the shape making use of the Preview switch and study the shape information to guarantee this is the best for you.
- In case the kind will not fulfill your needs, make use of the Seach area to find the right kind.
- Once you are certain the shape is acceptable, click on the Get now switch to find the kind.
- Choose the rates plan you would like and enter the required information and facts. Design your bank account and pay for an order using your PayPal bank account or credit card.
- Pick the data file format and acquire the lawful file design in your system.
- Complete, revise and print out and indicator the obtained Virginia Acknowledgment of Receipt of COBRA Notice.
US Legal Forms may be the greatest collection of lawful varieties in which you can discover a variety of file themes. Utilize the service to acquire appropriately-manufactured documents that follow condition specifications.
Form popularity
FAQ
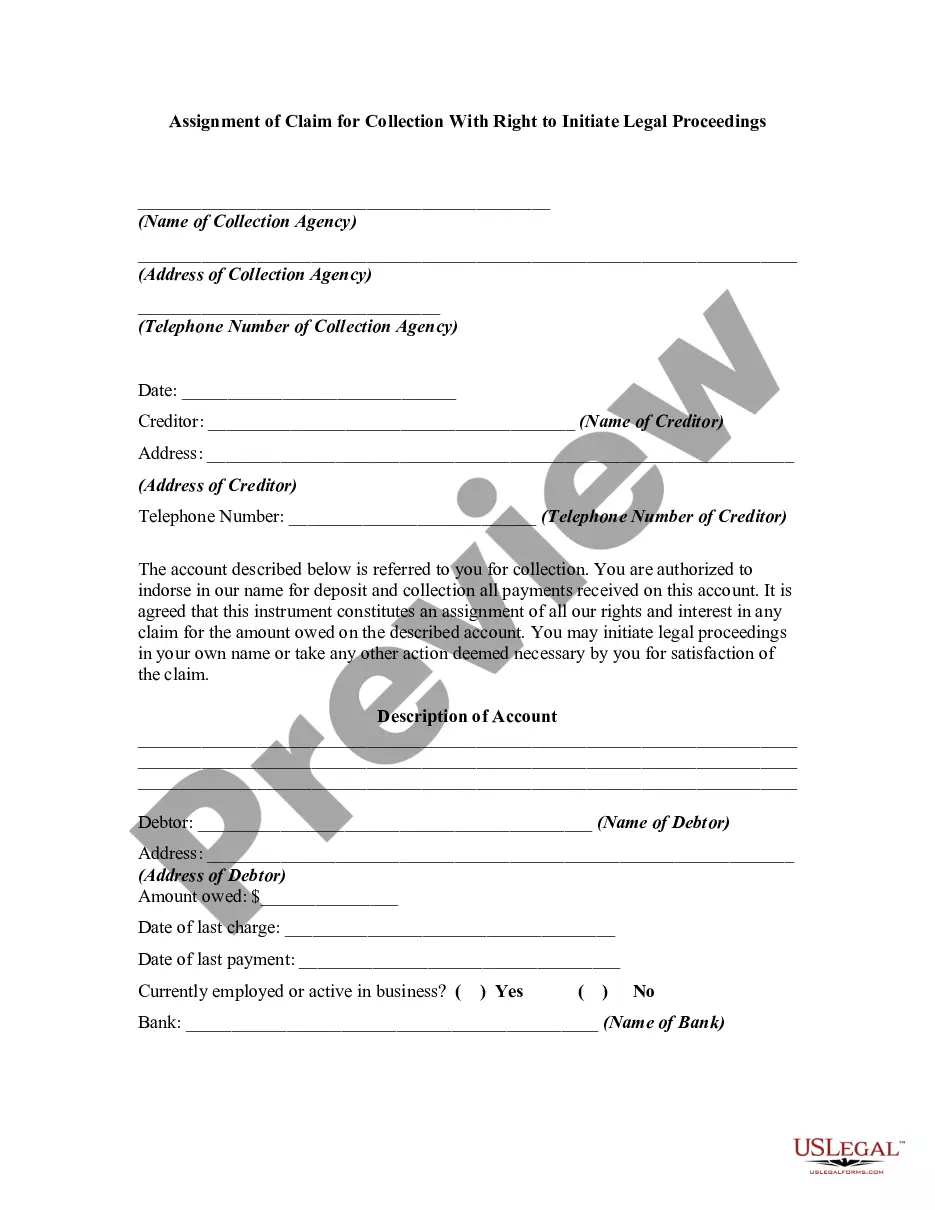
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Virginia mini-COBRA law provides for 12 months of continuation coverage, except in the case of terminations for cause. The employer is required provide an election form within 14 days after the date that coverage would otherwise terminate.
Nothing changes with your health insurance coverage, but now you are responsible for paying the full monthly premium. In addition, you also have to pay a 2% COBRA administration fee. COBRA costs an average of $599 per month.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
§ 15-409. The Virginia mini-COBRA law provides for 12 months of continuation coverage, except in the case of terminations for cause. The employer is required provide an election form within 14 days after the date that coverage would otherwise terminate.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
To be eligible for the continuation coverage, an individual must have been continuously insured under the group policy for the 3 months immediately before the termination of eligibility.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.