Virginia Qualifying Event Notice Information for Employer to Plan Administrator In Virginia, the Qualifying Event Notice serves as a critical communication tool between an employer and the plan administrator when certain events occur that may affect an employee's benefits under a group health plan. This detailed description will discuss the purpose, types, and key elements of the Virginia Qualifying Event Notice Information for Employers to Plan Administrators. The primary purpose of the Qualifying Event Notice is to notify the plan administrator of significant events that trigger changes or adjustments in an employee's health plan coverage. By promptly informing the plan administrator, employers ensure compliance with federal and state regulations and facilitate the smooth administration of a group health plan. There are several types of qualifying events that require employers to issue a Notice to the plan administrator in Virginia. These include, but are not limited to: 1. Termination of employment: When an employee's employment is terminated, they may become eligible for continued health benefits under COBRA (Consolidated Omnibus Budget Reconciliation Act). The Qualifying Event Notice should provide details about the termination, such as the employee's name, employment end date, and the reason for termination. 2. Reduction in hours: If an employee's hours are reduced, causing them to lose eligibility for the group health plan, the employer must notify the plan administrator. The Qualifying Event Notice should include the employee's name, the effective date of the reduction in hours, and any available alternative coverage options. 3. Divorce or legal separation: In cases where an employee's coverage is affected due to a divorce or legal separation, the employer is required to send a Qualifying Event Notice to the plan administrator. It should include the employee's name, the date of the divorce or legal separation, and any changes in the dependent coverage. 4. Death of an employee: When an employee passes away, their dependents may be eligible for continued health coverage under COBRA. The Qualifying Event Notice should specify the employee's name, date of death, and provide information about the continuation of coverage options for the eligible dependents. 5. Military leave: If an employee goes on military leave, they may elect to continue their health coverage under the Uniformed Services Employment and Reemployment Rights Act (SERRA). The Qualifying Event Notice should outline the employee's name, departure date for military duty, and the available health coverage options during their absence. When drafting a Qualifying Event Notice, certain essential elements should be included: a. Employer details: The notice must clearly identify the employer's name, address, and contact information. b. Employee details: The notice should contain the employee's full name, employment status, and relevant personal information to ensure accurate identification. c. Qualifying event details: Precise information regarding the qualifying event, such as the date it occurred, its nature, and the potential impact on the employee's health coverage. d. COBRA information: If the qualifying event triggers COBRA eligibility, the notice should provide a brief summary of the continuation coverage rights, election period, and premium payment details. e. Time frame: The notice must specify the deadline by which the employee or their dependents should respond to maintain their health coverage rights. It is crucial for employers to understand and comply with Virginia's Qualifying Event Notice requirements to avoid penalties and maintain smooth employee benefit administration. By promptly and accurately providing the necessary information to the plan administrator, employers actively support the well-being and continuity of their employees' health coverage.
Virginia Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Virginia Qualifying Event Notice Information For Employer To Plan Administrator?
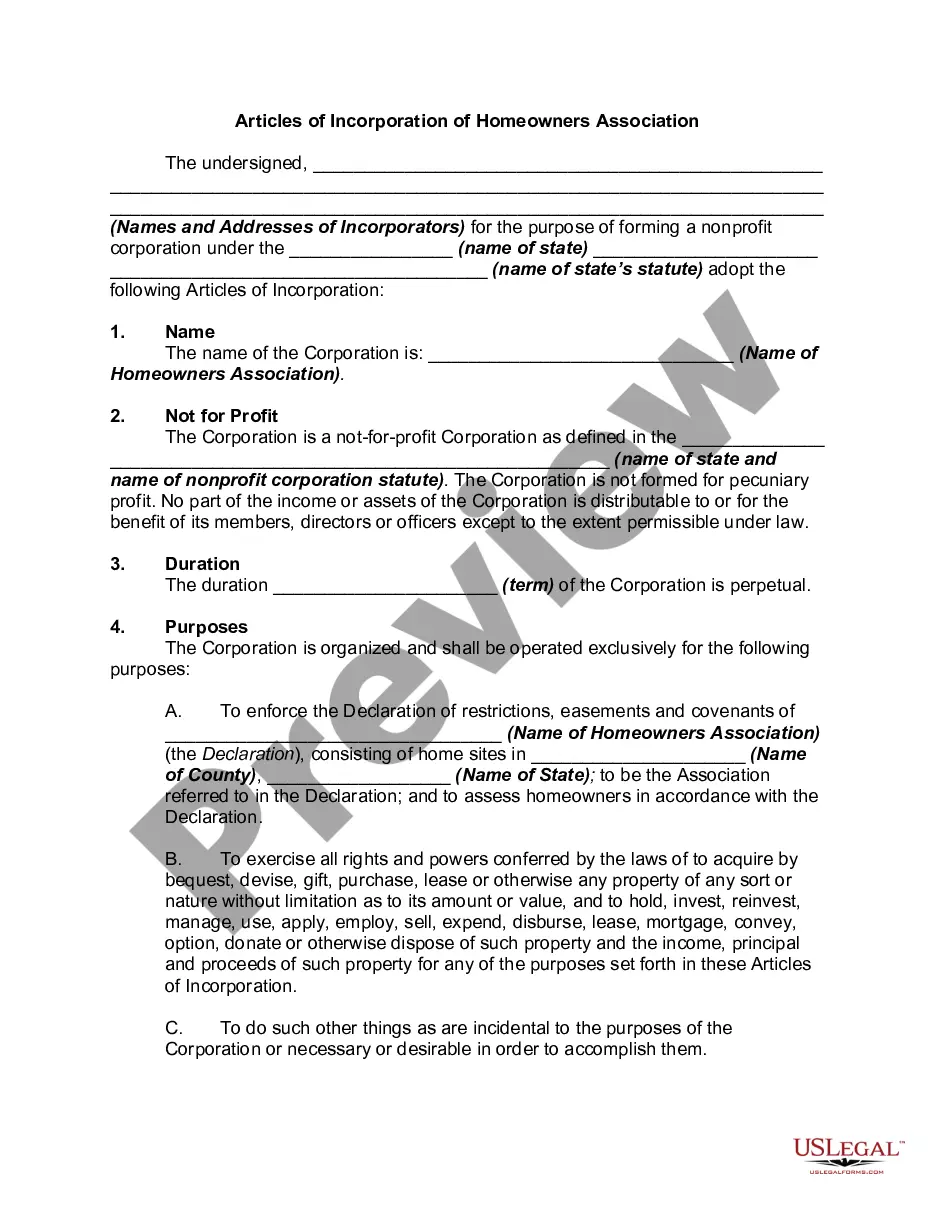
It is possible to spend time on the web attempting to find the lawful record template that meets the state and federal demands you want. US Legal Forms offers 1000s of lawful varieties that are reviewed by pros. You can actually down load or print the Virginia Qualifying Event Notice Information for Employer to Plan Administrator from our assistance.
If you have a US Legal Forms accounts, you are able to log in and then click the Down load option. Afterward, you are able to total, revise, print, or sign the Virginia Qualifying Event Notice Information for Employer to Plan Administrator. Every single lawful record template you purchase is the one you have forever. To get an additional backup of any acquired form, check out the My Forms tab and then click the related option.
If you are using the US Legal Forms web site initially, follow the simple directions below:
- Very first, make sure that you have chosen the best record template to the county/metropolis of your choice. Look at the form description to make sure you have picked out the correct form. If accessible, use the Review option to look through the record template too.
- If you want to locate an additional edition of your form, use the Lookup field to obtain the template that fits your needs and demands.
- Upon having identified the template you desire, simply click Get now to continue.
- Select the rates prepare you desire, type your accreditations, and sign up for a free account on US Legal Forms.
- Complete the financial transaction. You may use your credit card or PayPal accounts to purchase the lawful form.
- Select the file format of your record and down load it to your gadget.
- Make adjustments to your record if necessary. It is possible to total, revise and sign and print Virginia Qualifying Event Notice Information for Employer to Plan Administrator.
Down load and print 1000s of record layouts utilizing the US Legal Forms website, which provides the biggest assortment of lawful varieties. Use professional and condition-distinct layouts to tackle your business or specific demands.