Virgin Islands Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
US Legal Forms - one of the largest collections of legal documents in the United States - provides a broad array of legal document templates that you can download or print.
Using the platform, you can locate thousands of forms for business and personal use, organized by categories, states, or keywords. You can find the most recent versions of forms such as the Virgin Islands Affidavit of No Coverage by Another Group Health Plan in moments.
If you already hold a subscription, Log In and obtain the Virgin Islands Affidavit of No Coverage by Another Group Health Plan from the US Legal Forms library. The Download button will appear on each document you view. You can access all previously acquired forms in the My documents tab of your profile.
Make edits. Complete, modify, print, and sign the downloaded Virgin Islands Affidavit of No Coverage by Another Group Health Plan.
Every template you add to your account has no expiration date and is yours forever. So, to download or print another copy, simply go to the My documents section and click on the form you need. Access the Virgin Islands Affidavit of No Coverage by Another Group Health Plan with US Legal Forms, the most comprehensive collection of legal document templates. Utilize thousands of professional and state-specific templates that cater to your business or personal needs.
- If you wish to use US Legal Forms for the first time, here are straightforward steps to help you begin.
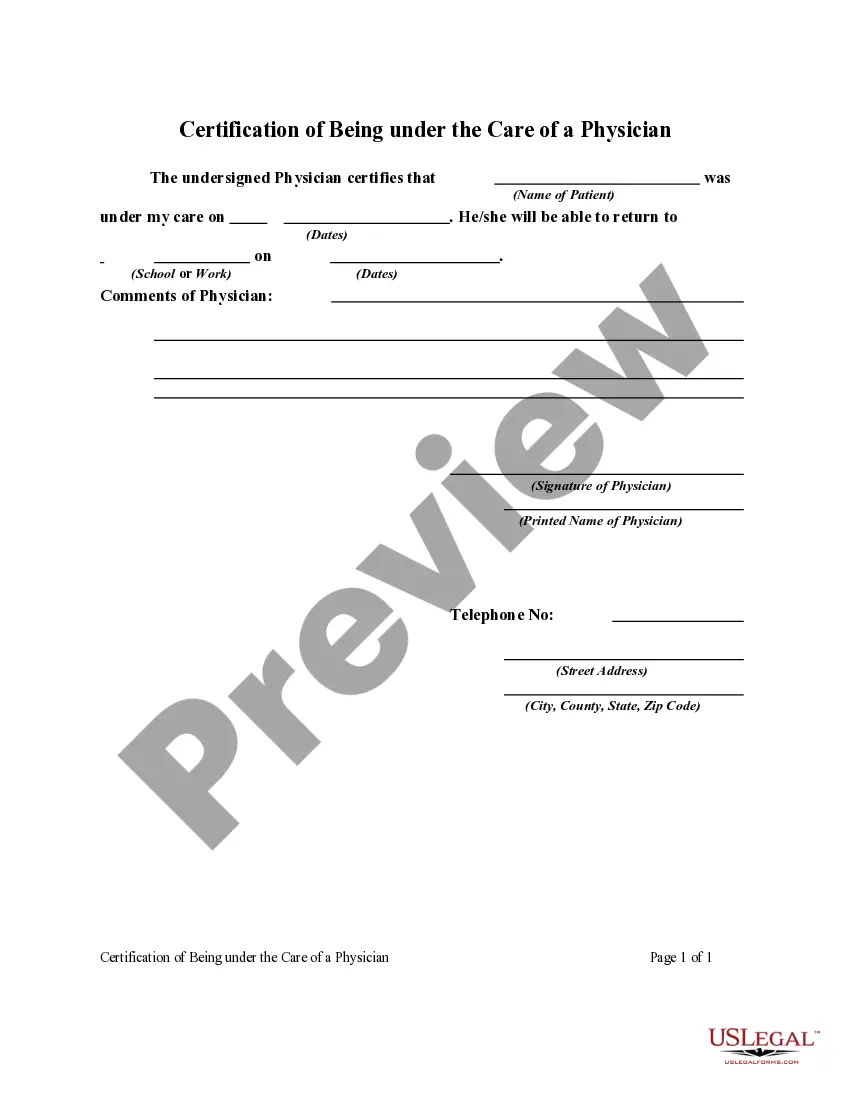
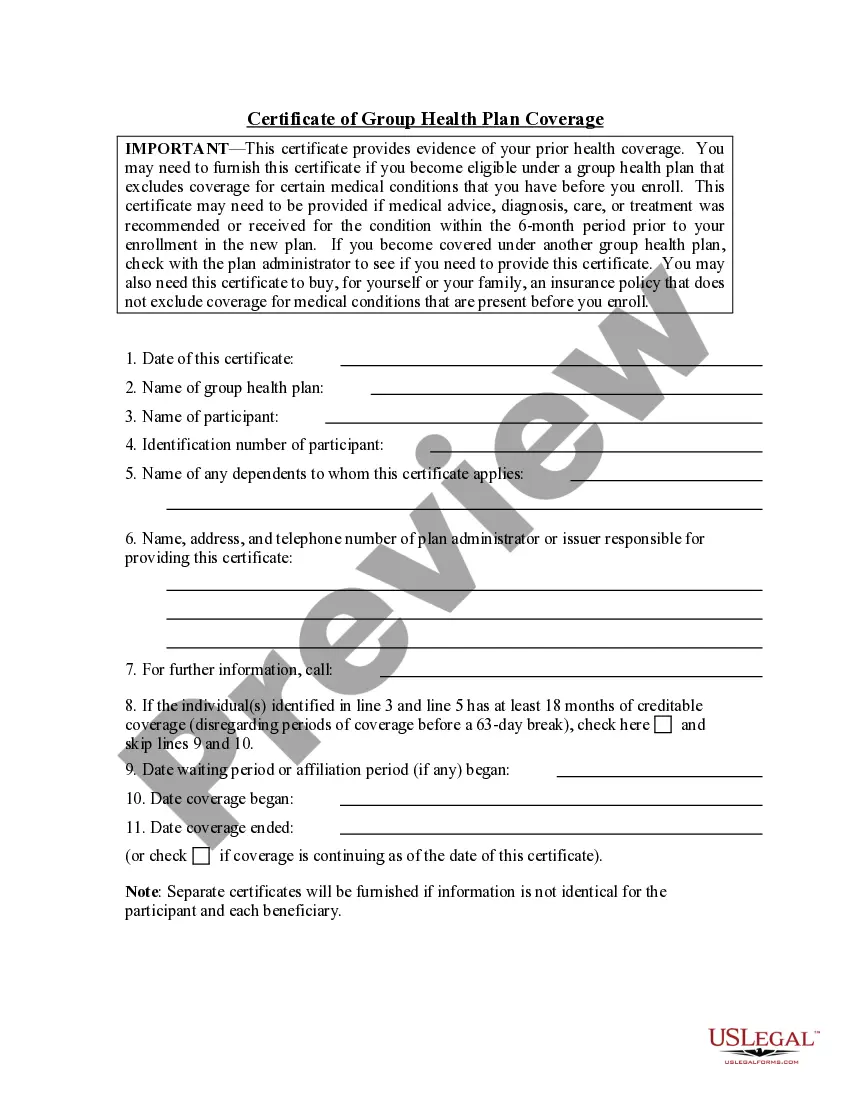
- Ensure you have selected the correct form for your city/county. Click on the Preview button to review the form's details. Examine the form description to confirm that you have selected the correct document.
- If the form does not meet your needs, utilize the Search box at the top of the screen to find the one that does.
- If you are satisfied with the document, confirm your choice by clicking the Buy now button. Then, choose the payment plan you prefer and enter your information to register for an account.
- Process the payment. Use your credit card or PayPal account to complete the purchase.
- Select the file format and download the document to your device.
Form popularity
FAQ
1. Inform the group insurance company: This is the first step for porting from your employer's health insurance plan to an individual one. You must inform the insurer at least 30-45 days before your last day of employment in the same company.
The purpose of the coordination of benefits (COB) provision is to avoid duplication of benefit payments and over insurance when an individual is covered under more than one group health plan.
If you fall ill or get hurt while visiting the U.S. Virgin Islands, your health insurance may cover your care. But if you need special medical transportation to a hospital or back to your home (repatriation), you may be out of luck.
What is the contract called that is issued to an employer for a Group Medical Insurance plan? (An employer would be a possible applicant and contract policyholder of a single master contract or master policy for group health benefits.)
When can a group health policy renewal be denied according to the Health Insurance Portability and Accountability Act (HIPAA)? When contribution or participation rules have been violated. Mark continues working after the age of 65 and is covered through his employer's group health plan.
When group health insurance is being replaced, ongoing claims under the former policy must continue under the new policy, overriding any preexisting condition exclusion.
The Coordination of Benefits (COB) provision applies when a person has health care coverage under more than one Plan. Plan is defined below. The order of benefit determination rules govern the order in which each Plan will pay a claim for benefits.
However, the following individuals are NOT eligible to participate in Section 125 Cafeteria Plan, Flexible Spending Account (FSA), or Premium Only Plan (POP), or any of its qualified benefits: More than 2% shareholder of an S-corporation, or any of its family members, Sole proprietor, Partner in a partnership, or.
Disadvantages of Health Insurance PolicyHealth insurance policy can be very costly even for those that have a health insurance plan through their employers. Costs may be so high that many end up struggling to make payments. This can be quite challenging for those who have low incomes or are self-employed.