Vermont Complaint regarding Group Insurance Contract
Description
How to fill out Complaint Regarding Group Insurance Contract?
Are you presently in a scenario where you need documents for either business or personal purposes almost every day.
There are numerous legal document templates accessible online, but finding reliable ones is challenging.
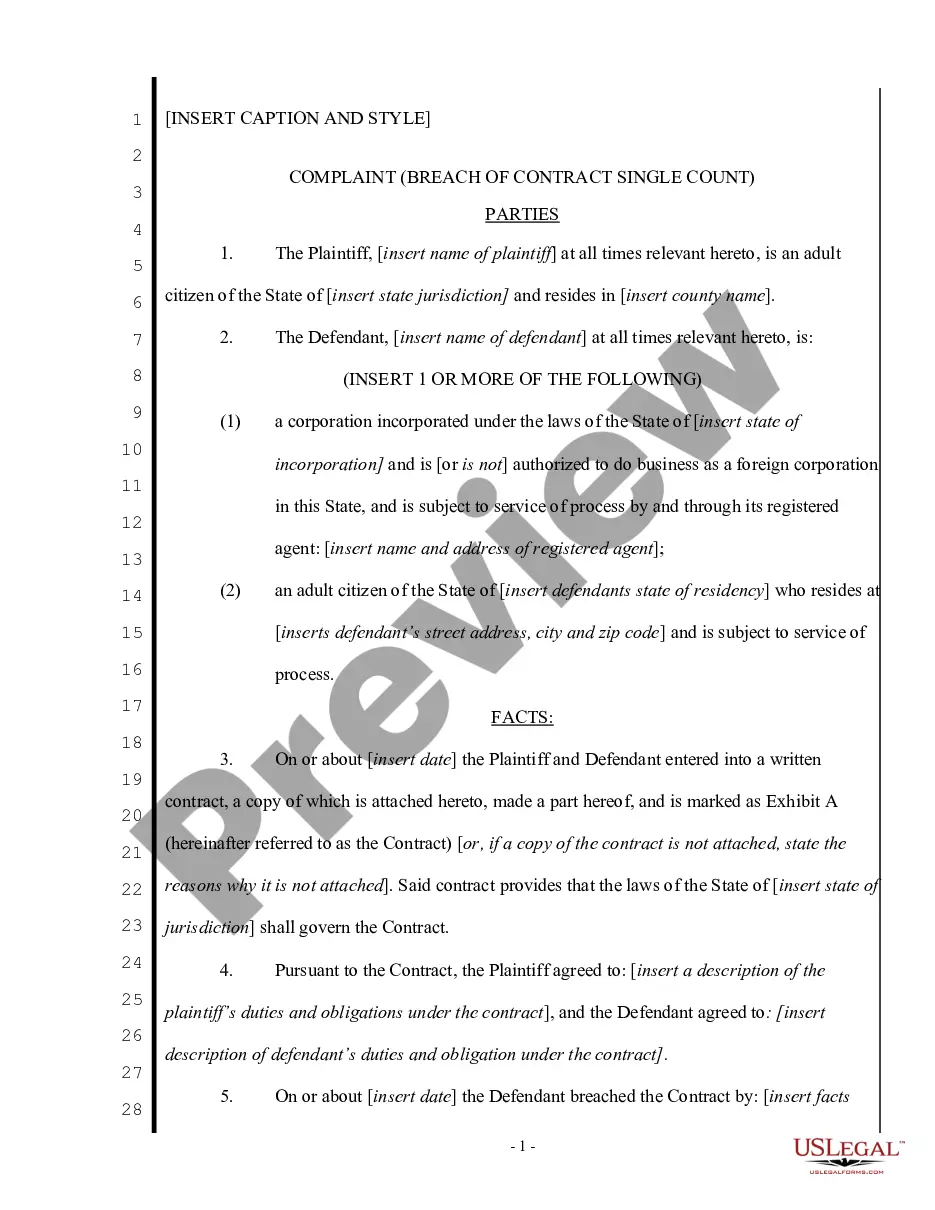
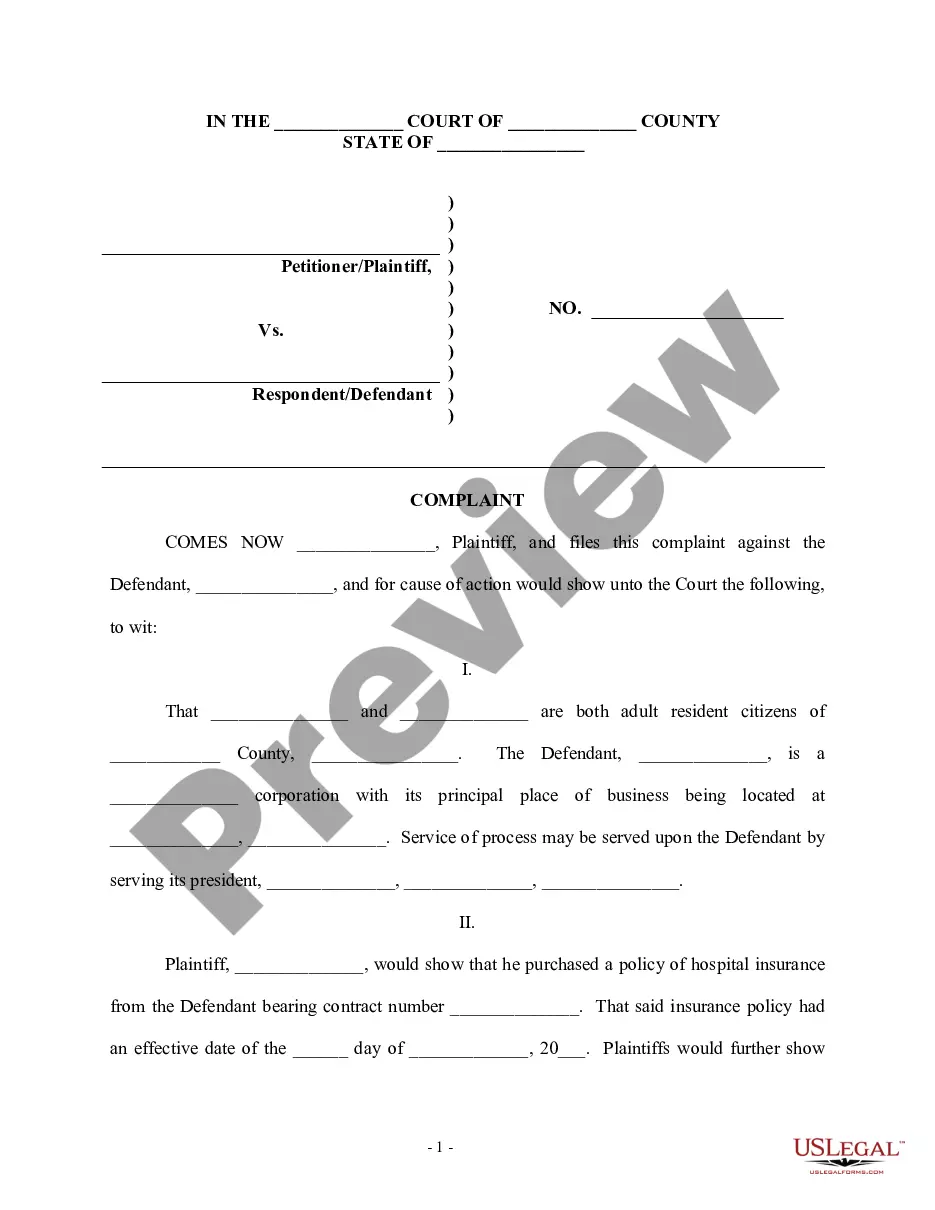
US Legal Forms offers a wide array of form templates, including the Vermont Complaint regarding Group Insurance Contract, which are designed to comply with state and federal regulations.
Once you find the correct form, click Buy now.
Choose the pricing plan you prefer, complete the required information to create your account, and pay for your order using your PayPal or credit card. Select a convenient document format and download your copy. Access all the document templates you have purchased in the My documents section. You can obtain an additional copy of the Vermont Complaint regarding Group Insurance Contract at any time, if necessary. Just click the needed form to download or print the document template. Make use of US Legal Forms, the most comprehensive selection of legal forms, to save time and avoid errors. This service provides professionally crafted legal document templates that can be utilized for various purposes. Create an account on US Legal Forms and start simplifying your life.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the Vermont Complaint regarding Group Insurance Contract template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and ensure it is for the correct state/region.
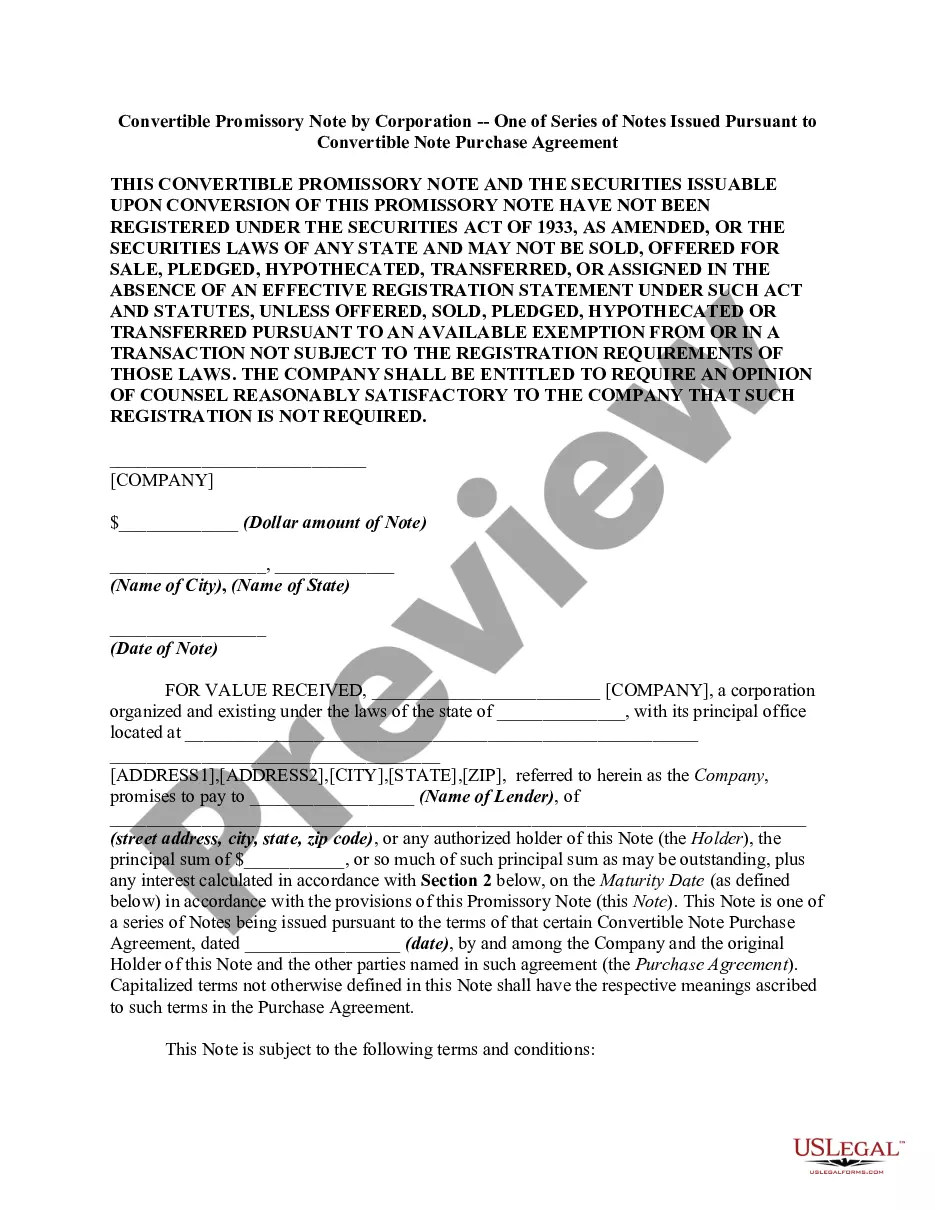
- Utilize the Preview button to review the document.
- Verify the details to confirm you have selected the right form.
- If the form does not meet your needs, use the Search field to locate the form that suits your requirements.
Form popularity
FAQ
Types of Insurance Fraud False or inflated theft repair claim. Owner ?give up? (false stolen car report) ?Jump in? (someone not in vehicle at time of accident) Staged accident. Intentional damage claim. Falsifying the date or circumstances of an accident to get coverage. Rate evasion.
Ask a third party such as an ombudsman to help with your dispute. File a complaint with your state department of insurance, which regulates insurance activity and insurer compliance with state laws and regulations. Seek arbitration if that is an option in your policy. File a legal claim against the insurer in court.
You can call your state's insurance department. If none of this helps, you can try an out-of-court settlement because most likely, once you've hired an attorney and they contact your insurance company, the dispute will be settled out of court.
Your right to appeal You may ask your insurance company to conduct a full and fair review of its decision. If the case is urgent, your insurance company must speed up this process. External review: You have the right to take your appeal to an independent third party for review. This is called an external review.
If you intend to seek compensation in your car accident claim, then you have the right to negotiate for more money. You will be, through your attorney, negotiating with the insurance company, and specifically, the claims adjuster, for the money you are entitled to.
All insurance policies sold in Vermont are reviewed and approved by the Insurance Division to ensure they provide protections mandated by Vermont law. The Division conducts annual and periodic audits of health insurance plans to ensure compliance with Vermont regulations.
Information To Include in Your Letter Give the basics. Tell your story. Tell the company how you want to resolve the problem. Be reasonable. File your complaint. Your Address. Your City, State, Zip Code. [Your email address, if sending by email] Date.
Call us at 800-649-2424. For over three decades, the Vermont Attorney General and UVM have worked together to help Vermont consumers and businesses. Find our consumer complaint form here.