Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation is an important document that provides employees with crucial information regarding the availability of continuation coverage under certain circumstances. This notice is typically issued by the employer or plan administrator to inform employees about their options when continuation coverage is not accessible. Here are some relevant keywords and terms associated with the Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: 1. Vermont Continuation Coverage: This term refers to the continuation of health insurance coverage under Vermont state law when certain events, such as termination or reduction of working hours, occur. 2. Employee Benefits: This phrase encompasses the various fringe benefits, including health insurance, that employees receive as part of their employment. 3. Plan Administrator: This refers to the person or entity responsible for managing the employee benefits plan, including the issuance of necessary notices and information like the Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation. 4. Unavailability of Continuation: This phrase denotes situations where an employee is unable to continue their health insurance coverage due to specific circumstances, such as the employer discontinuing the plan or the employee's ineligibility for coverage. 5. COBRA Coverage: COBRA (Consolidated Omnibus Budget Reconciliation Act) is a federal law that allows employees to continue their health insurance coverage temporarily after certain qualifying events. However, the Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation specifies situations when COBRA coverage may not be available. Different Types of Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: 1. Ineligibility Notice: This notice is issued when an employee does not meet the criteria to be eligible for continuation coverage. It provides detailed information about the reasons for ineligibility and alternative options available to the employee. 2. Plan Discontinuation Notice: This type of notice is sent to employees when their employer decides to discontinue the health insurance plan altogether. It informs them of the plan's termination and outlines alternative coverage options they may explore. 3. Limited Coverage Notice: This notice is issued when an employee's coverage period has expired or will expire soon. It indicates that continuation coverage is not available beyond a specific timeframe, and the employee should pursue alternative health insurance options. In summary, the Vermont Employer — Plan Administrator Notice to Employee of Unavailability of Continuation is a crucial document that outlines the unavailability of continuation coverage under specific circumstances. It ensures that employees are fully aware of their rights, options, and responsibilities regarding their health insurance coverage in Vermont.
Vermont Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Vermont Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
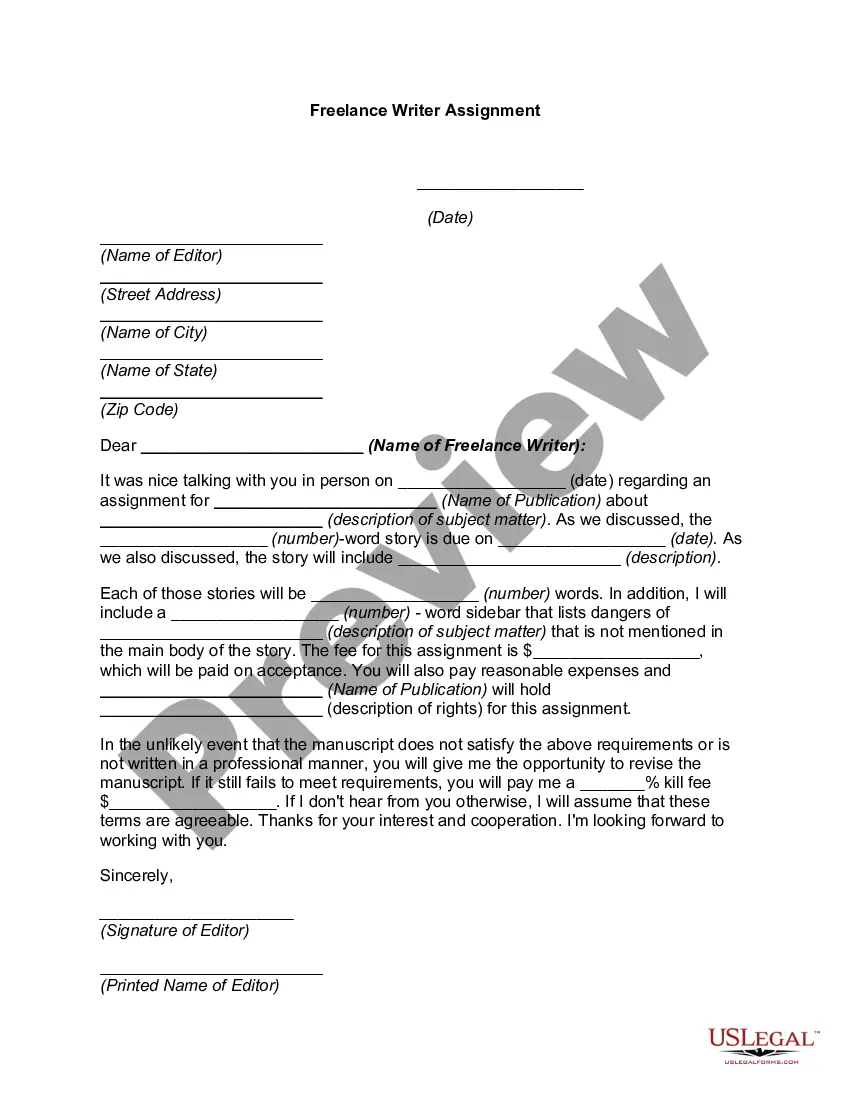
Are you within a place the place you require papers for possibly business or person uses virtually every time? There are a variety of legal file layouts available on the Internet, but locating types you can rely on isn`t easy. US Legal Forms provides 1000s of develop layouts, much like the Vermont Employer - Plan Administrator Notice to Employee of Unavailability of Continuation, that happen to be written to meet federal and state specifications.
When you are presently knowledgeable about US Legal Forms web site and possess your account, merely log in. Next, it is possible to obtain the Vermont Employer - Plan Administrator Notice to Employee of Unavailability of Continuation web template.
If you do not have an accounts and want to begin to use US Legal Forms, adopt these measures:
- Obtain the develop you want and make sure it is to the right metropolis/area.
- Utilize the Preview button to examine the form.
- Look at the outline to ensure that you have selected the right develop.
- In the event the develop isn`t what you`re looking for, make use of the Lookup industry to discover the develop that meets your needs and specifications.
- When you discover the right develop, simply click Purchase now.
- Choose the rates program you want, fill out the desired details to create your account, and pay money for an order using your PayPal or charge card.
- Choose a convenient paper structure and obtain your duplicate.
Locate every one of the file layouts you might have bought in the My Forms food selection. You can get a further duplicate of Vermont Employer - Plan Administrator Notice to Employee of Unavailability of Continuation any time, if needed. Just go through the needed develop to obtain or print the file web template.
Use US Legal Forms, probably the most comprehensive assortment of legal forms, to save time as well as steer clear of faults. The services provides skillfully manufactured legal file layouts that can be used for a variety of uses. Create your account on US Legal Forms and start producing your way of life easier.
Form popularity
FAQ
How long will COBRA continuation coverage last? When loss of coverage due to end of employment or a reduction in hours of employment, coverage generally may be continued for up to a total of 18 months.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
Time employee has to apply: 30 days after termination; 60 days if employer fails to give notice. Employers affected: All employers who offer group health insurance.
If you work 35 hours or more or your earnings exceed your weekly benefit amount plus your disregarded earnings, you will be considered fully employed and will not be entitled to receive benefit for that week.
Under COBRA, you and your family have the right to remain on whatever health plan your former employer has for up to 18 months. You must continue paying the full premium, which includes both your former employer's share and your share plus a 2 percent administrative fee.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
In the private sector it's called COBRA. In the federal government it's called Temporary Continuation of Coverage. In both cases it's a way to remain in an employer-sponsored health insurance program when you leave that employer for a time, although at a higher cost.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
B. Eighteen (18) months for a Dependent who is a Qualified Beneficiary unless a second Qualifying Event occurs within that eighteen-month period entitling that Dependent to an additional eighteen (18) months; C.