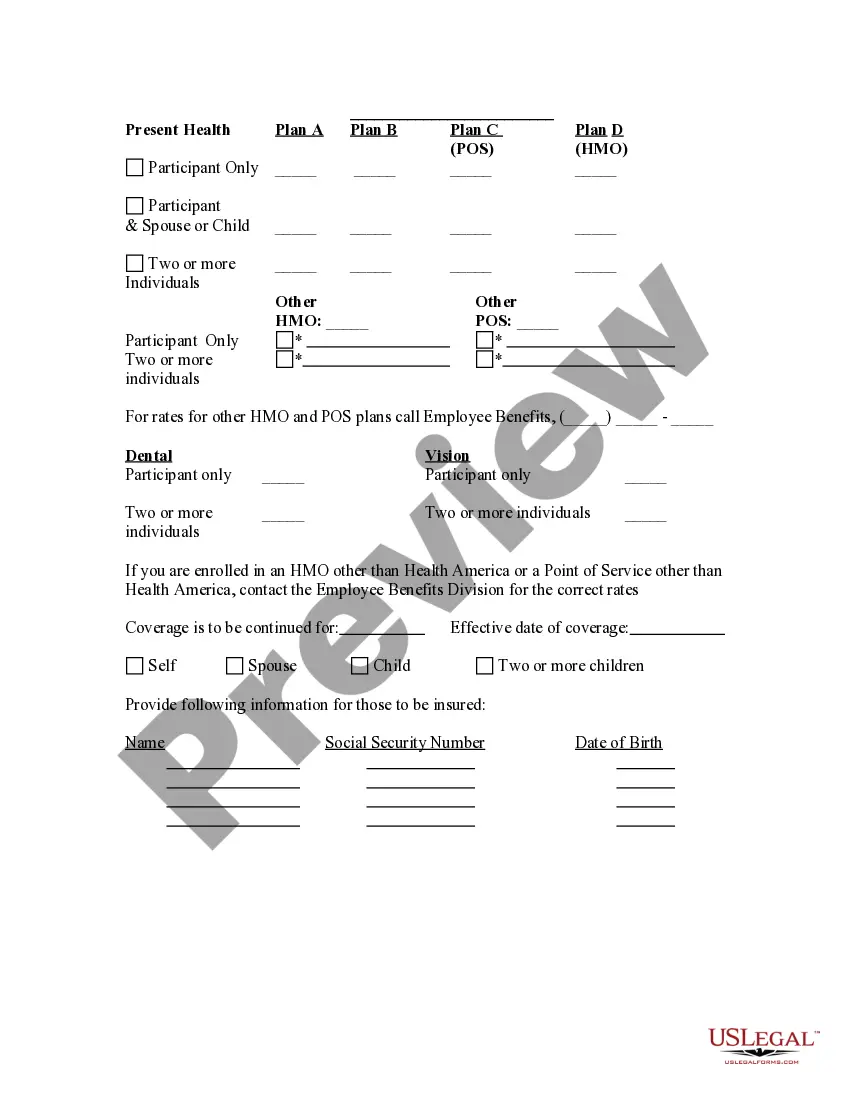
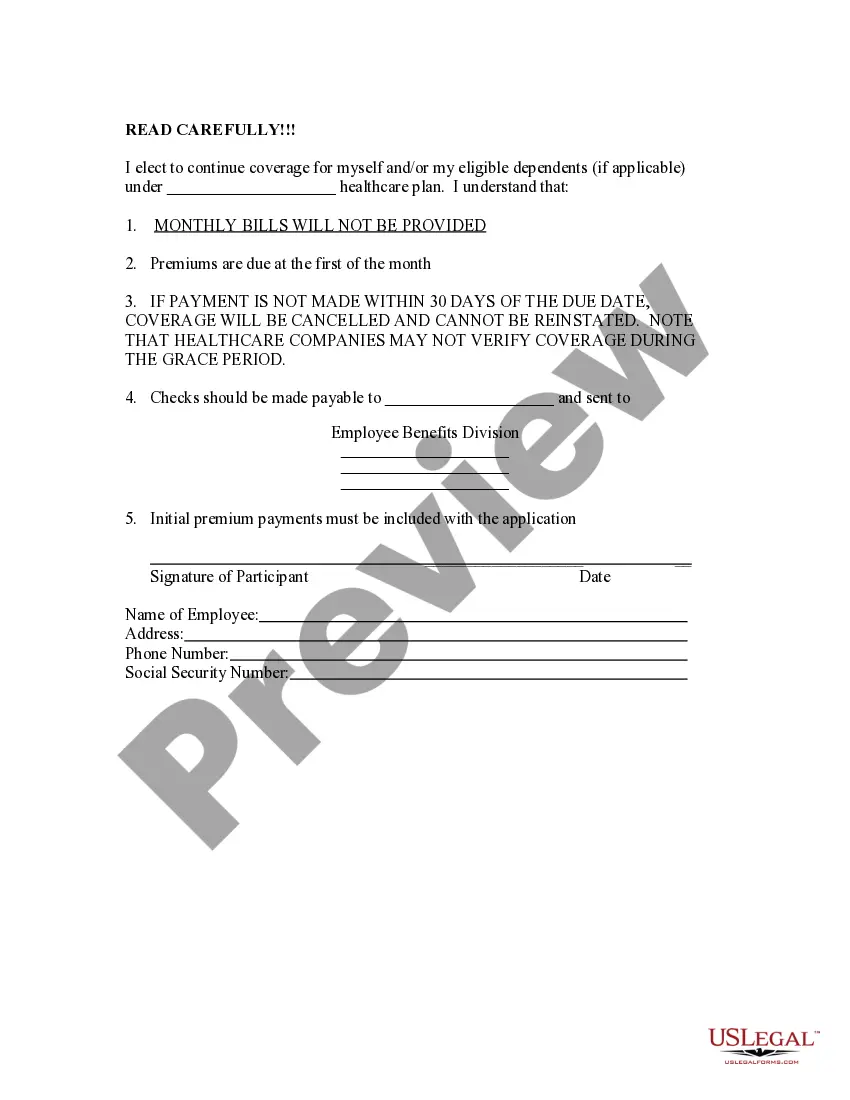
The Washington Election Form for Continuation of Benefits, also known as COBRA, is a crucial document that allows eligible individuals to elect continued health insurance coverage after experiencing a qualifying event. COBRA refers to the Consolidated Omnibus Budget Reconciliation Act, a federal law that provides workers and their families the right to keep their group health plan coverage for a limited period. This form is specific to Washington state and is used to ensure compliance with the state's COBRA regulations. The Washington Election Form for Continuation of Benefits — COBRA is a comprehensive document that outlines the terms and conditions of continued coverage, allowing employees and their dependents to make informed decisions about their medical insurance. It includes various sections that require detailed information, ensuring accurate record-keeping and efficient processing of the continuation benefits. Some important keywords relevant to the Washington Election Form for Continuation of Benefits — COBRA include: 1. Qualifying event: Refers to specific situations that make an employee or their dependents eligible for COBRA coverage, such as termination of employment, reduction in work hours, or death of the covered employee. This keyword highlights the trigger for possible continuation benefits. 2. Health insurance coverage: Emphasizes that the Washington Election Form for Continuation of Benefits — COBRA is specifically designed for maintaining medical insurance. It serves as a proof of election and serves to initiate the continuation coverage process outlined in the form. 3. Eligibility criteria: Details the requirements that individuals must meet to qualify for COBRA coverage. This could include factors like length of previous coverage, not being eligible for Medicare, or being a dependent beneficiary. 4. Duration of coverage: Specifies the maximum duration for which an individual can maintain COBRA coverage. In Washington state, it typically extends up to 18 months, although there may be provisions for extensions in certain circumstances. 5. Dependent information: Requests identifying details of dependents who will be covered under the continuation plan. This section ensures proper enrollment and accurate billing for extended coverage. It's important to note that while the Washington Election Form for Continuation of Benefits — COBRA is the standard form used in the state, there may be additional variations or supplemental forms specific to certain organizations or insurance providers. These forms may contain additional fields or provisions to tailor the COBRA continuation benefits to their respective plans and policies.
Washington Election Form for Continuation of Benefits - COBRA
Description
How to fill out Washington Election Form For Continuation Of Benefits - COBRA?
You are able to commit several hours on the web searching for the lawful document template that fits the state and federal requirements you need. US Legal Forms provides a huge number of lawful kinds which are analyzed by specialists. You can actually acquire or print the Washington Election Form for Continuation of Benefits - COBRA from the assistance.
If you already have a US Legal Forms profile, you may log in and click the Obtain switch. After that, you may comprehensive, revise, print, or indicator the Washington Election Form for Continuation of Benefits - COBRA. Every single lawful document template you purchase is yours forever. To obtain one more version of any bought kind, visit the My Forms tab and click the corresponding switch.
If you use the US Legal Forms site initially, stick to the simple guidelines below:
- Initial, make certain you have selected the correct document template for the region/area of your choosing. Browse the kind information to ensure you have chosen the right kind. If readily available, utilize the Review switch to appear from the document template too.
- If you want to discover one more edition of the kind, utilize the Look for industry to get the template that meets your needs and requirements.
- Upon having located the template you want, click on Purchase now to carry on.
- Pick the prices strategy you want, type in your qualifications, and register for an account on US Legal Forms.
- Complete the deal. You may use your charge card or PayPal profile to pay for the lawful kind.
- Pick the formatting of the document and acquire it for your gadget.
- Make alterations for your document if needed. You are able to comprehensive, revise and indicator and print Washington Election Form for Continuation of Benefits - COBRA.
Obtain and print a huge number of document themes while using US Legal Forms site, which offers the greatest selection of lawful kinds. Use skilled and condition-distinct themes to take on your small business or specific requirements.