Wyoming Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
If you wish to total, download, or printing authorized file themes, use US Legal Forms, the most important assortment of authorized types, that can be found on the web. Utilize the site`s simple and handy lookup to get the files you want. Various themes for business and personal uses are categorized by groups and suggests, or keywords and phrases. Use US Legal Forms to get the Wyoming Summary of Rights and Obligations under COBRA in just a handful of click throughs.
Should you be presently a US Legal Forms buyer, log in in your accounts and click the Acquire switch to find the Wyoming Summary of Rights and Obligations under COBRA. You can also access types you previously acquired in the My Forms tab of the accounts.
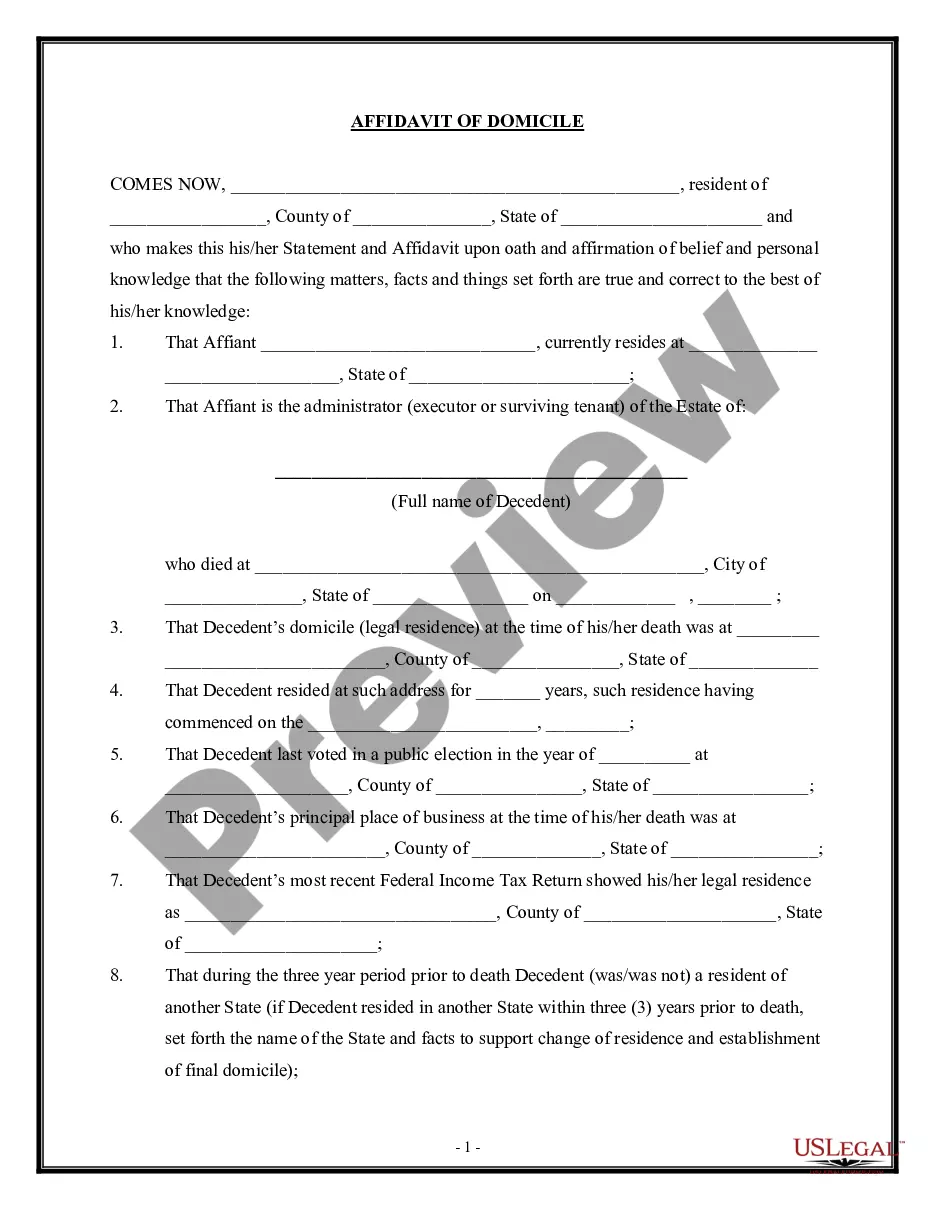
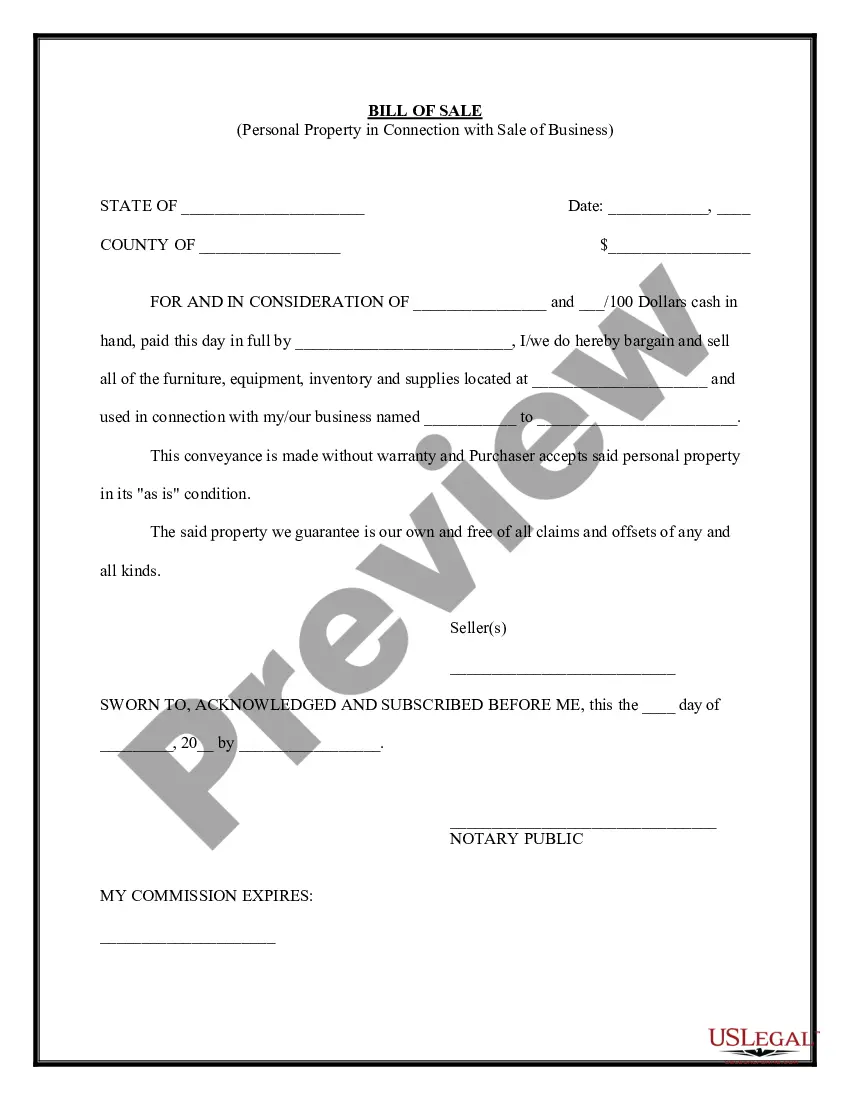
If you work with US Legal Forms initially, follow the instructions listed below:
- Step 1. Make sure you have selected the form for your right area/nation.
- Step 2. Take advantage of the Preview method to examine the form`s articles. Don`t forget about to see the outline.
- Step 3. Should you be unsatisfied using the type, use the Research area on top of the screen to get other models of your authorized type design.
- Step 4. Once you have discovered the form you want, select the Purchase now switch. Select the costs prepare you favor and put your qualifications to sign up to have an accounts.
- Step 5. Method the purchase. You may use your bank card or PayPal accounts to finish the purchase.
- Step 6. Choose the structure of your authorized type and download it in your device.
- Step 7. Complete, edit and printing or signal the Wyoming Summary of Rights and Obligations under COBRA.
Each and every authorized file design you get is your own permanently. You have acces to every type you acquired inside your acccount. Click the My Forms area and pick a type to printing or download once more.
Be competitive and download, and printing the Wyoming Summary of Rights and Obligations under COBRA with US Legal Forms. There are thousands of specialist and condition-particular types you can use for your business or personal requires.
Form popularity
FAQ
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,