The Wyoming Model COBRA Continuation Coverage Election Notice is a crucial document provided to employees who are eligible for COBRA continuation coverage in the state of Wyoming. COBRA stands for Consolidated Omnibus Budget Reconciliation Act, which is a federal law that allows individuals to continue their health insurance coverage after experiencing certain qualifying events that would otherwise cause them to lose their coverage. This notice is designed to inform employees about their rights, options, and responsibilities when it comes to electing COBRA continuation coverage. It is a comprehensive document that outlines all the necessary information regarding eligibility, enrollment periods, coverage details, and payment requirements. The Wyoming Model COBRA Continuation Coverage Election Notice includes essential keywords such as "COBRA continuation coverage," "eligibility," "enrollment periods," "coverage details," and "payment requirements." These keywords help readers understand the document's purpose and content. Additionally, there are two main types of Wyoming Model COBRA Continuation Coverage Election Notices: 1. Initial Notice: This notice is provided to employees and their dependents when they first become eligible for COBRA continuation coverage. It explains their rights and options, including the opportunity to continue their existing group health insurance coverage for a limited period of time. 2. Qualifying Event Notice: This notice is sent to individuals who experience a qualifying event that triggers their eligibility for COBRA continuation coverage. Qualifying events can include termination of employment, reduction in work hours, divorce or legal separation, or the death of the covered employee. The notice informs individuals of their right to elect COBRA continuation coverage within a specific period of time following the qualifying event. In conclusion, the Wyoming Model COBRA Continuation Coverage Election Notice is a critical document that provides important information to employees and their dependents regarding their rights and options for continuing health insurance coverage under COBRA. It ensures that individuals receive the necessary details to make informed decisions about their healthcare coverage during significant life events.
Wyoming Model COBRA Continuation Coverage Election Notice
Description
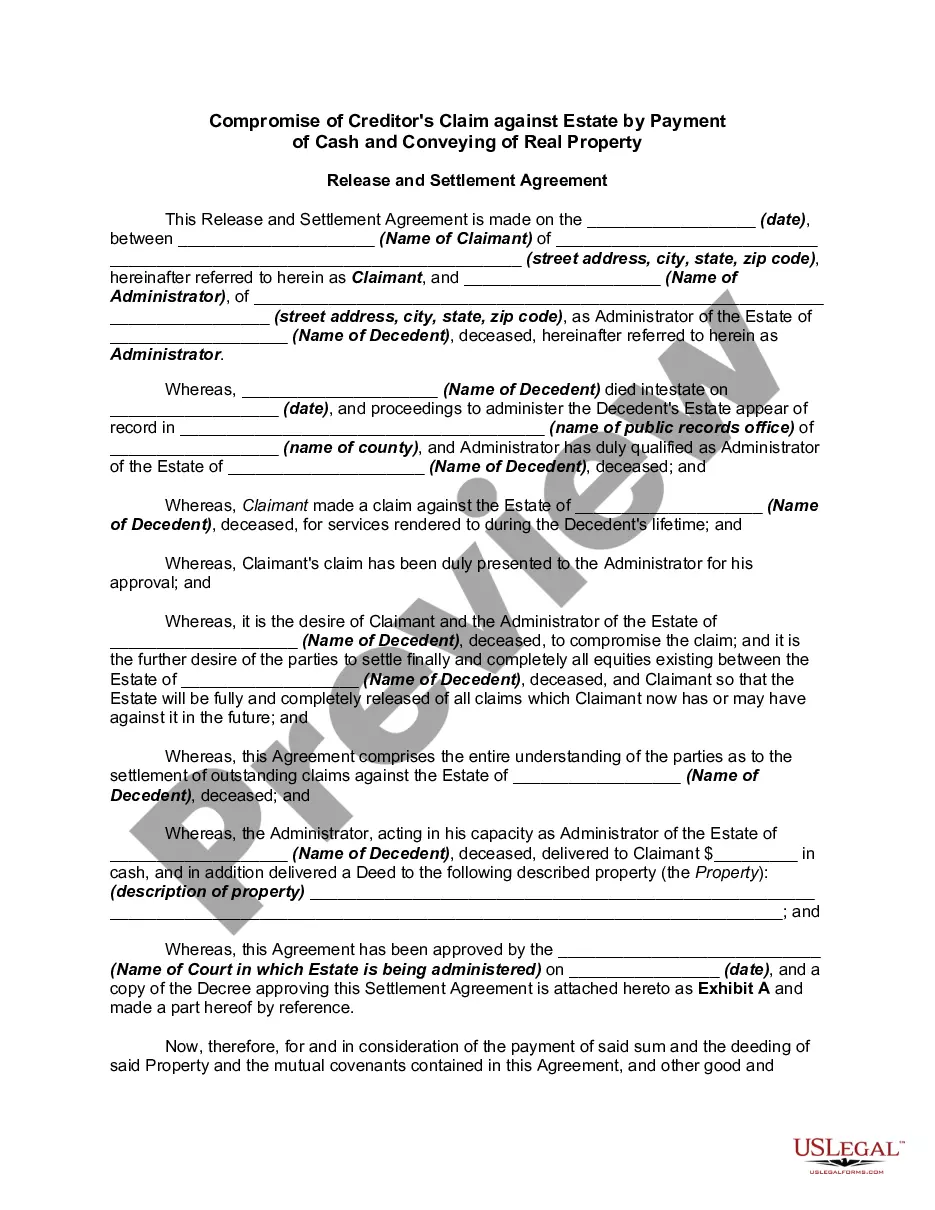
How to fill out Wyoming Model COBRA Continuation Coverage Election Notice?
Choosing the right legitimate papers template could be a have a problem. Obviously, there are a lot of layouts available online, but how can you get the legitimate form you need? Use the US Legal Forms web site. The support delivers a large number of layouts, including the Wyoming Model COBRA Continuation Coverage Election Notice, that you can use for enterprise and personal requirements. All of the forms are checked by specialists and satisfy state and federal specifications.
In case you are presently registered, log in to your profile and click the Download button to find the Wyoming Model COBRA Continuation Coverage Election Notice. Utilize your profile to search from the legitimate forms you possess ordered previously. Proceed to the My Forms tab of your profile and obtain an additional duplicate in the papers you need.
In case you are a fresh customer of US Legal Forms, here are basic directions that you can adhere to:
- Very first, make sure you have chosen the proper form to your town/region. You can look over the shape making use of the Preview button and look at the shape outline to make certain it will be the right one for you.
- In the event the form fails to satisfy your expectations, take advantage of the Seach field to find the correct form.
- When you are sure that the shape is proper, go through the Purchase now button to find the form.
- Select the pricing plan you would like and type in the required information and facts. Create your profile and pay money for an order with your PayPal profile or charge card.
- Opt for the submit file format and download the legitimate papers template to your system.
- Total, edit and produce and sign the acquired Wyoming Model COBRA Continuation Coverage Election Notice.
US Legal Forms is definitely the largest collection of legitimate forms for which you can find a variety of papers layouts. Use the service to download skillfully-produced files that adhere to state specifications.