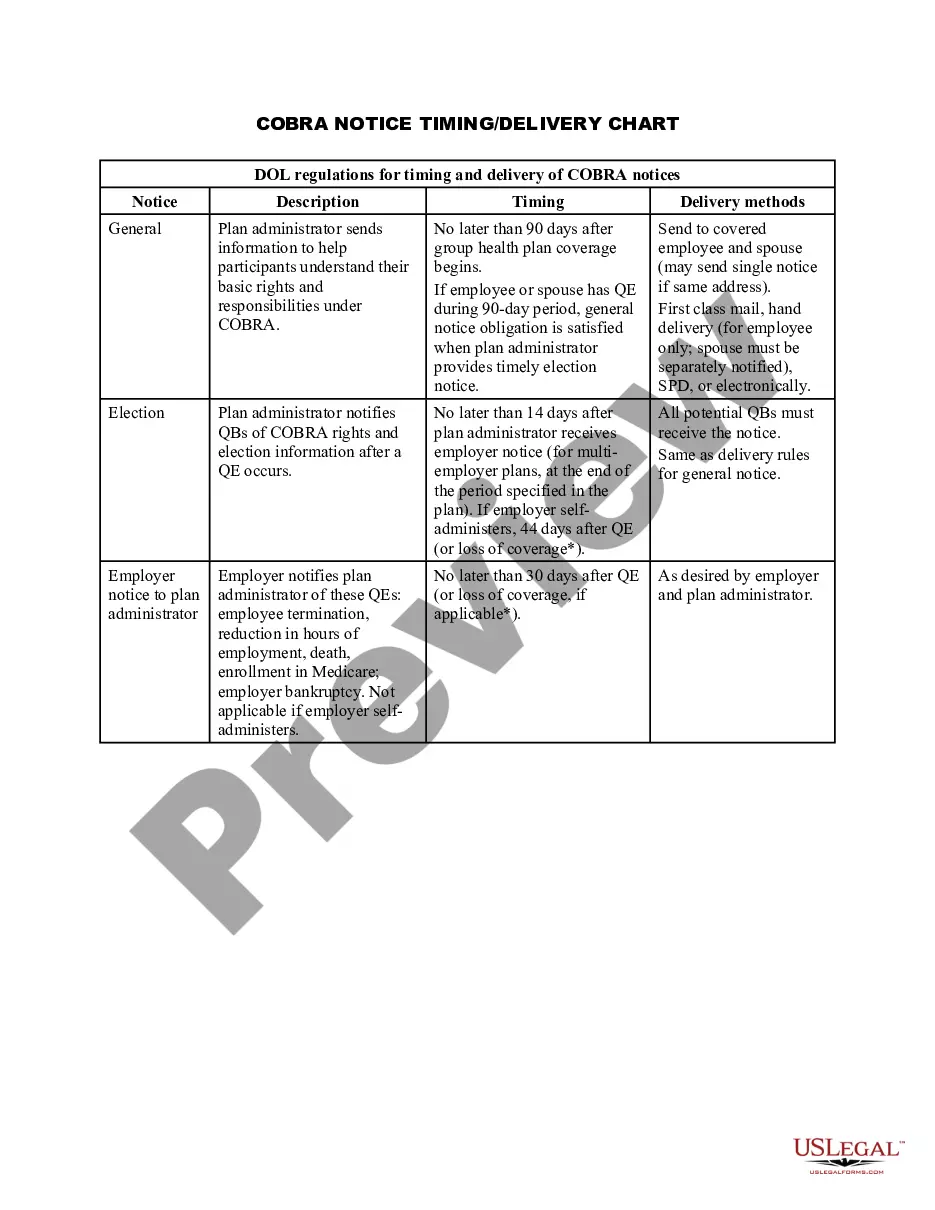
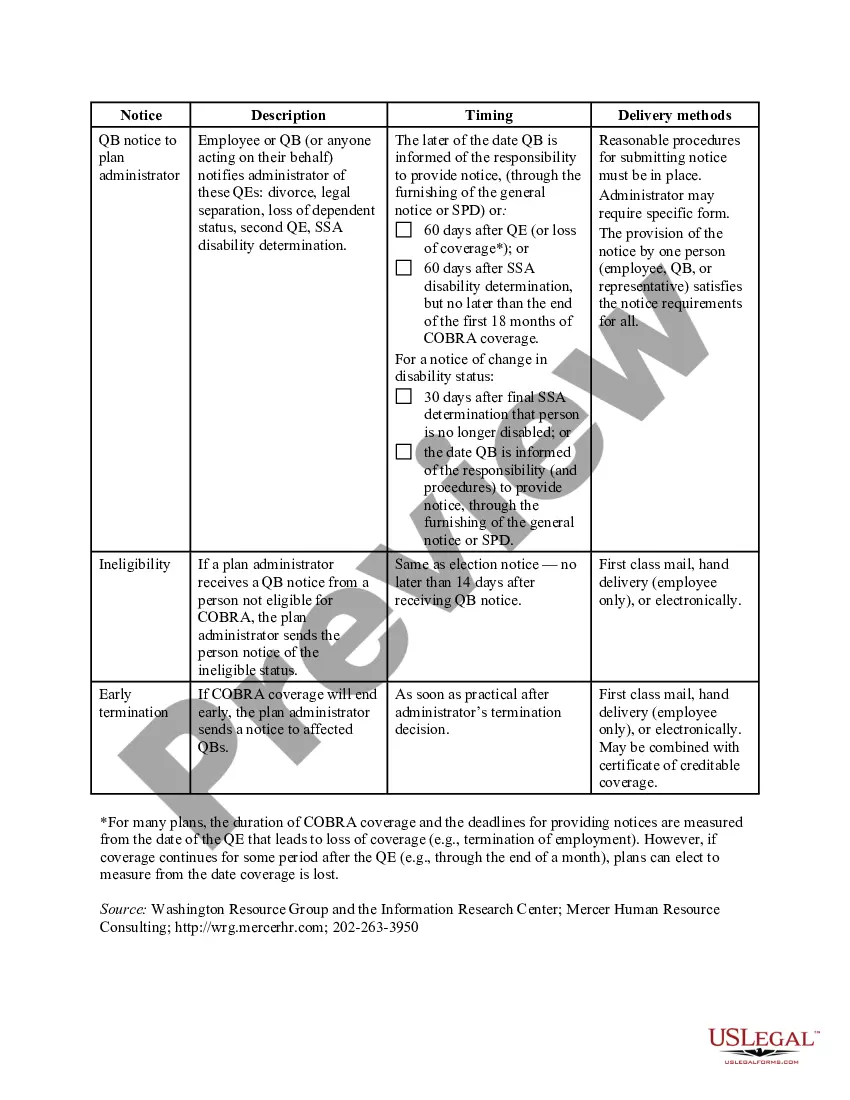
Title: Understanding the Wyoming COBRA Notice Timing Delivery Chart: Key Information and Types Introduction: The Wyoming COBRA Notice Timing Delivery Chart is a crucial document that outlines the timeline and specific requirements for employers and employees in relation to COBRA (Consolidated Omnibus Budget Reconciliation Act) notices. This article aims to provide a detailed description of the Wyoming COBRA Notice Timing Delivery Chart, including its importance, components, and potential variations or types. Key Points: 1. Importance of COBRA Notices: COBRA notices play a vital role in informing employees and their qualified beneficiaries about their rights to continue healthcare coverage when there is a qualifying event that would otherwise result in a loss of coverage. Compliance with COBRA regulations is essential for employers to avoid legal penalties and ensure employees' access to continued healthcare coverage. 2. Understanding the Wyoming COBRA Notice Timing Delivery Chart: The Wyoming COBRA Notice Timing Delivery Chart serves as a helpful reference tool for employers in the state to understand the specific timeframes for delivering COBRA notices to eligible individuals. It outlines the specific deadlines that employers must adhere to while providing COBRA information to employees and qualified beneficiaries. 3. Components of the Notice Timing Delivery Chart: The Notice Timing Delivery Chart typically consists of several key components, including: a. Initial Notice: This refers to the notice provided to employees and their qualified beneficiaries upon commencement of group health plan coverage. b. Qualifying Event Notice: This notice is given to individuals within a specific timeframe after a qualifying event, such as termination of employment or reduction of hours. c. Election Notice: This notice provides individuals with an opportunity to elect COBRA coverage within a defined period. d. Premium Payment Notice: Employers are required to notify individuals about the payment terms, due dates, and consequences of non-payment related to COBRA coverage. 4. Variations or Types of Wyoming COBRA Notice Timing Delivery Chart: While the Wyoming COBRA Notice Timing Delivery Chart provides a general guideline, it is important to note that the chart may vary depending on individual circumstances. Some specific types or variations may include: a. Federal COBRA Coverage: Employers with 20 or more employees are subject to federal COBRA regulations, which generally apply to employees in the private sector. b. State Continuation Coverage: Wyoming state law mandates employers with fewer than 20 employees to offer continuation coverage, often referred to as mini-COBRA. This may have distinct notice timing and delivery requirements. Conclusion: The Wyoming COBRA Notice Timing Delivery Chart acts as a crucial tool for employers, enabling them to comply with COBRA regulations by providing timely and accurate notices to eligible individuals. Understanding the chart's components and potential variations is essential to ensure compliance and guarantee the continuation of healthcare coverage for qualified beneficiaries. Remember, consulting legal experts, COBRA administrators, or state-specific resources will provide further clarification regarding the Wyoming COBRA Notice Timing Delivery Chart.
Wyoming COBRA Notice Timing Delivery Chart
Description
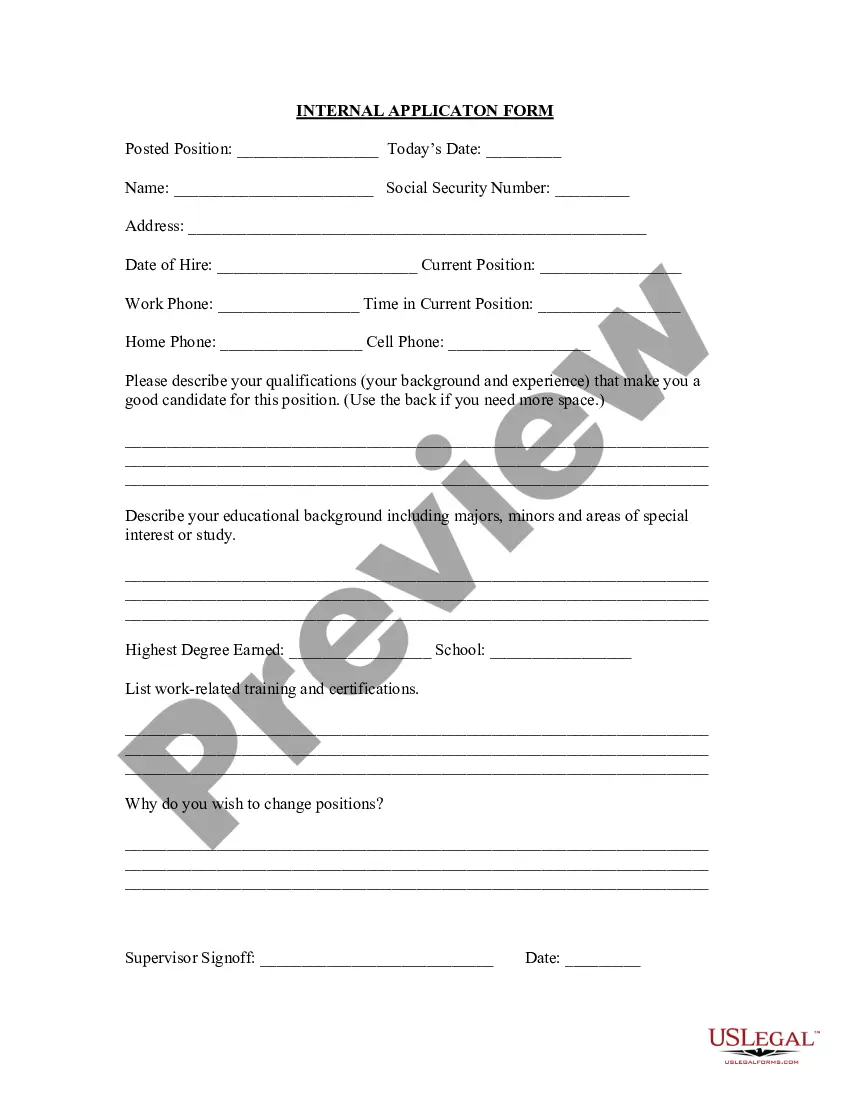
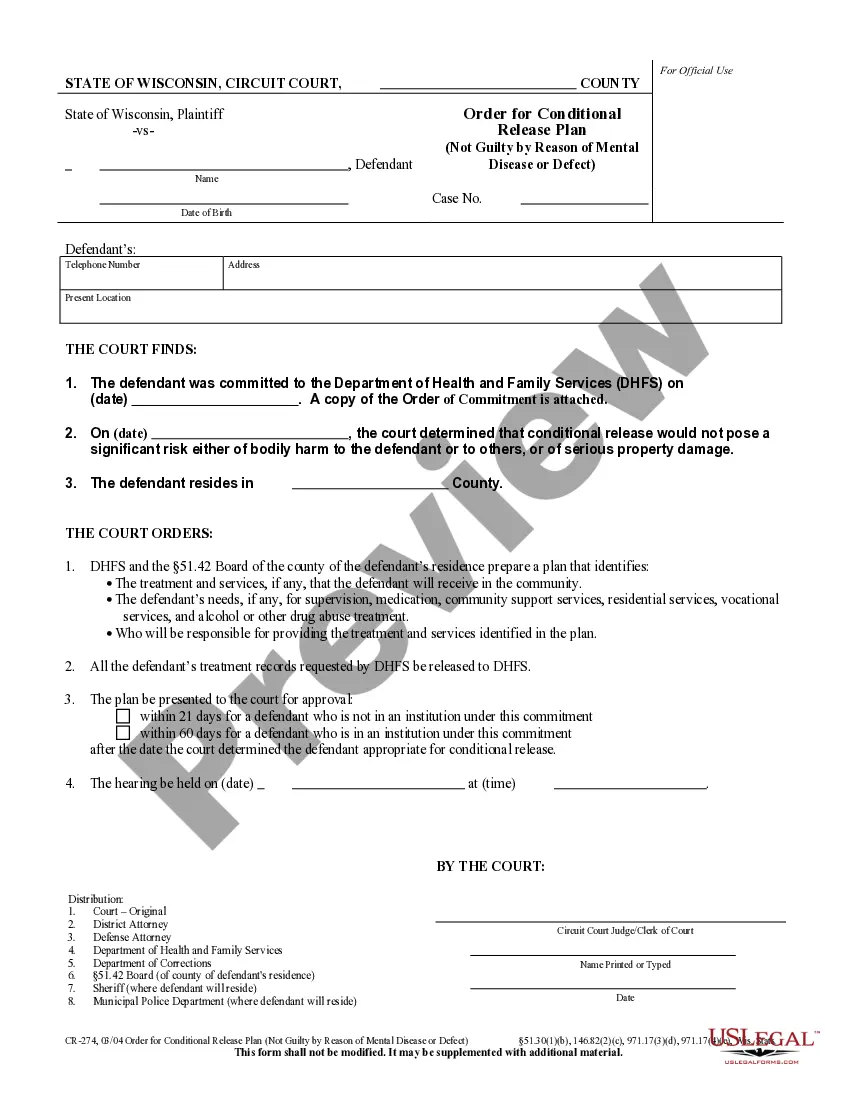
How to fill out Wyoming COBRA Notice Timing Delivery Chart?
You may spend several hours on the Internet attempting to find the legitimate papers design that meets the federal and state needs you need. US Legal Forms offers 1000s of legitimate kinds that happen to be evaluated by pros. You can easily download or produce the Wyoming COBRA Notice Timing Delivery Chart from our service.
If you already possess a US Legal Forms accounts, you can log in and click the Down load key. Following that, you can complete, change, produce, or signal the Wyoming COBRA Notice Timing Delivery Chart. Each legitimate papers design you purchase is your own property for a long time. To get one more duplicate associated with a obtained form, go to the My Forms tab and click the corresponding key.
If you use the US Legal Forms web site initially, keep to the straightforward instructions beneath:
- Very first, make sure that you have selected the proper papers design for your county/town of your choosing. Browse the form outline to make sure you have chosen the proper form. If available, take advantage of the Review key to look from the papers design too.
- If you wish to locate one more edition from the form, take advantage of the Research field to discover the design that fits your needs and needs.
- Once you have identified the design you want, click Get now to proceed.
- Select the rates strategy you want, key in your accreditations, and register for a merchant account on US Legal Forms.
- Total the transaction. You can utilize your Visa or Mastercard or PayPal accounts to pay for the legitimate form.
- Select the structure from the papers and download it to your gadget.
- Make alterations to your papers if necessary. You may complete, change and signal and produce Wyoming COBRA Notice Timing Delivery Chart.
Down load and produce 1000s of papers templates while using US Legal Forms website, which provides the greatest assortment of legitimate kinds. Use specialist and express-distinct templates to handle your small business or person needs.
Form popularity
FAQ
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA continuation coverage may be terminated if we don't receive timely payment of the premium. What is the grace period for monthly COBRA premiums? After election and initial payment, qualified beneficiaries have a 30-day grace period to make monthly payments (that is, 30 days from the due date).
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
COBRA allows a 30-day grace period. If your premium payment is not received within the 30-day grace period, your coverage will automatically be terminated without advance warning. You will receive a termination letter at that time to notify you of a lapse in your coverage due to non-payment of premiums.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Are there penalties for failing to provide a COBRA notice? Yes, and the penalties can be substantial. Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
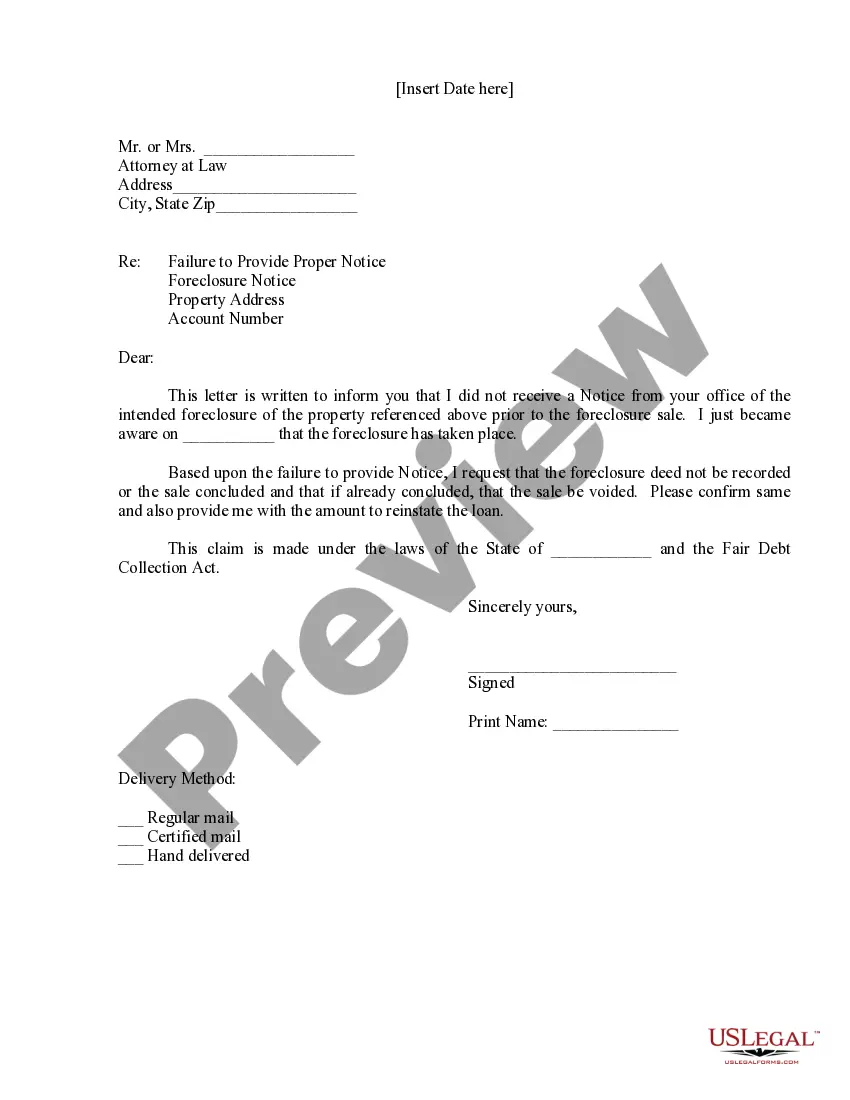
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.