Centennial Colorado Request for Utilization Review for Workers' Compensation is a formal document that individuals or their employers submit to the relevant authorities to seek a review of the medical treatment they have received or plan to receive related to a work-related injury or illness. This request aims to ensure that the proposed medical services are appropriate and necessary for the injured employee's recovery. Keywords: Centennial Colorado, request for utilization review, workers' compensation, medical treatment, work-related injury, illness, review, appropriate, necessary, recovery. Different Types of Centennial Colorado Request for Utilization Review for Workers' Compensation: 1. Initial Utilization Review Request: This type of request is submitted by an injured employee or their employer when they initially seek medical treatment for a work-related injury or illness. It serves as the first step in the review process to ensure that the proposed treatment plan aligns with the state's workers' compensation guidelines. 2. Pre-Authorization Review Request: This type of request is made by an injured worker or their healthcare provider to seek approval for specific medical services or treatment before they are administered. This ensures that the proposed treatment is necessary and related to the work-related injury or illness. 3. Additional or Continued Treatment Review Request: If an injured employee or their healthcare provider determines that additional or continued treatment is required beyond the initially authorized services, this request is submitted to seek approval for further medical care. It provides detailed justification and medical evidence to support the need for extended treatment. 4. Disputed Treatment Review Request: In cases where the injured employee, employer, or insurance carrier disagrees with a decision made by the workers' compensation insurance company regarding the necessity or appropriateness of a certain medical treatment, this request is filed. It initiates a review process to resolve the dispute and reach a fair resolution. 5. Second Opinion Review Request: If an injured employee or their healthcare provider believes that a second opinion from another medical professional is necessary, they can submit this request. It seeks authorization to consult with another healthcare provider to obtain an alternative perspective on the proposed medical treatment. Centennial Colorado Request for Utilization Review for Workers' Compensation plays a crucial role in ensuring that injured employees receive appropriate medical care and that employers and insurance carriers comply with the state's workers' compensation regulations. It is an essential mechanism for maintaining fairness, transparency, and efficiency in the provision of medical services for work-related injuries and illnesses.
Centennial Colorado Request for Utilization Review for Workers' Compensation
Description
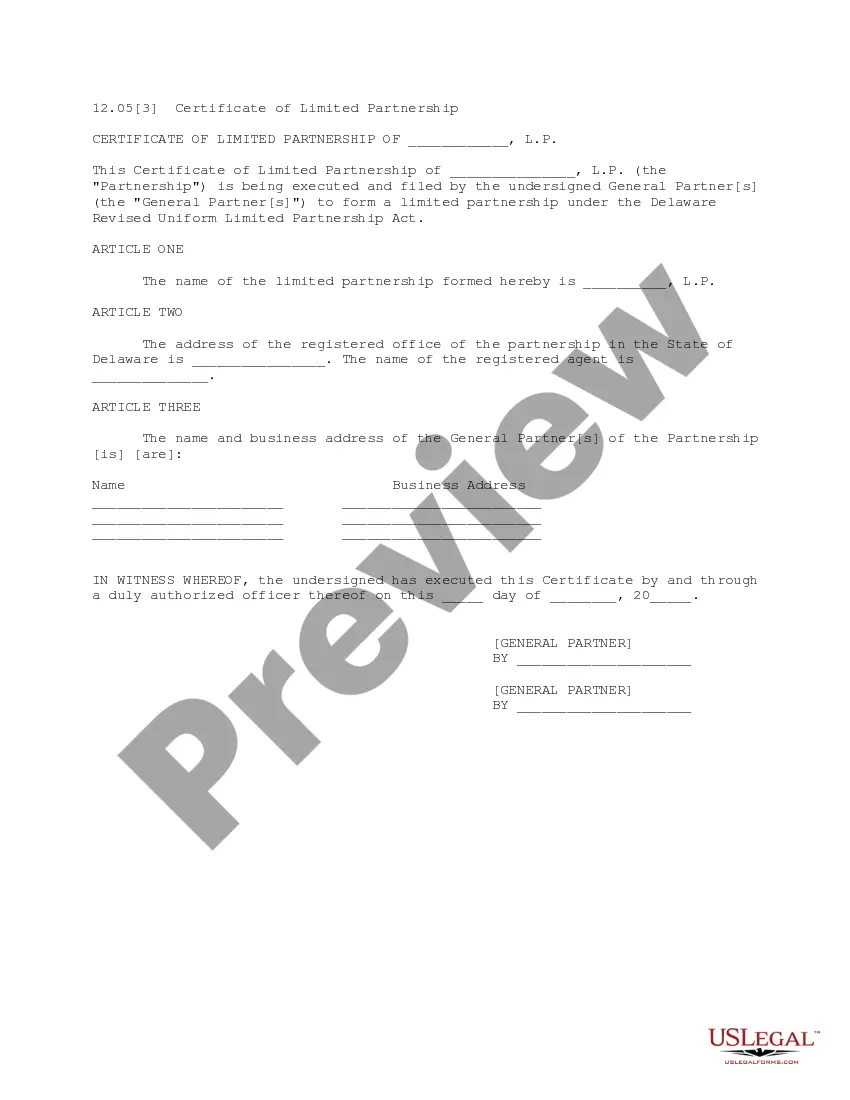
How to fill out Centennial Colorado Request For Utilization Review For Workers' Compensation?
If you are searching for a valid form template, it’s extremely hard to choose a better platform than the US Legal Forms site – one of the most considerable online libraries. Here you can find a huge number of form samples for company and individual purposes by categories and regions, or keywords. Using our advanced search function, getting the most recent Centennial Colorado Request for Utilization Review for Workers' Compensation is as elementary as 1-2-3. Additionally, the relevance of every record is proved by a team of expert lawyers that regularly check the templates on our website and update them according to the newest state and county regulations.
If you already know about our platform and have an account, all you need to receive the Centennial Colorado Request for Utilization Review for Workers' Compensation is to log in to your user profile and click the Download button.
If you use US Legal Forms the very first time, just follow the guidelines listed below:
- Make sure you have chosen the sample you want. Look at its information and make use of the Preview function (if available) to explore its content. If it doesn’t meet your needs, use the Search field near the top of the screen to get the proper record.
- Affirm your choice. Click the Buy now button. Next, choose the preferred subscription plan and provide credentials to sign up for an account.
- Process the purchase. Utilize your bank card or PayPal account to complete the registration procedure.
- Receive the template. Indicate the format and save it on your device.
- Make changes. Fill out, modify, print, and sign the obtained Centennial Colorado Request for Utilization Review for Workers' Compensation.
Each template you save in your user profile has no expiry date and is yours permanently. You always have the ability to gain access to them via the My Forms menu, so if you need to have an extra duplicate for enhancing or creating a hard copy, you may return and download it again at any time.
Take advantage of the US Legal Forms professional library to get access to the Centennial Colorado Request for Utilization Review for Workers' Compensation you were looking for and a huge number of other professional and state-specific templates on one platform!