Fort Collins Colorado Request for Utilization Review for Workers' Compensation is a crucial process that enables employers and insurers to effectively manage and control medical treatment expenses related to work-related injuries. This review ensures that the provided medical care is necessary, appropriate, and aligned with the standards outlined by the Colorado Division of Workers' Compensation. By using relevant keywords, we can provide a detailed description of this process. The Fort Collins Colorado Request for Utilization Review for Workers' Compensation is primarily initiated when an injured worker requires medical treatment following a workplace injury or illness. This request aims to determine the medical necessity and the appropriateness of the proposed treatment plan. Keywords related to this process may include: 1. Utilization Review: The utilization review process involves an assessment of medical treatment plans proposed by healthcare providers to ensure they align with guidelines and standards set forth by the Colorado Division of Workers' Compensation. 2. Workers' Compensation: Workers' compensation refers to a system that provides medical treatment, wage replacement, and other benefits to employees who have been injured or become ill as a result of their job duties. This request is specific to workers' compensation cases in Fort Collins, Colorado. 3. Medical Necessity: Medical necessity refers to the requirement that the proposed treatment or service is appropriate and essential in treating the worker's injury or illness. The utilization review determines if the recommended treatment aligns with this criterion. 4. Treatment Plan: A treatment plan is a comprehensive outline of the medical interventions, therapies, and procedures recommended by the healthcare provider to facilitate the injured worker's recovery. This plan undergoes scrutiny during the utilization review process. Different types of Fort Collins Colorado Requests for Utilization Review for Workers' Compensation may include: 1. Initial Treatment Review: This type of review focuses on the medical treatment plan proposed by the healthcare provider for the immediate management of the worker's injury or illness. 2. Ongoing Treatment Review: As the injured worker's condition progresses, healthcare providers may propose subsequent treatments or therapies. This review assesses the continued necessity and appropriateness of the ongoing treatment plan. 3. Pre-Authorization Review: In some cases, medical treatment may require pre-authorization, especially if it involves certain procedures, surgeries, or medications. This review evaluates whether the requested treatment is essential before approval is granted. 4. Second Opinion Review: Occasionally, a second opinion from another healthcare provider may be sought to validate the initial treatment plan. This review determines the most appropriate course of action based on multiple professional opinions. In conclusion, the Fort Collins Colorado Request for Utilization Review for Workers' Compensation is a critical component of managing and controlling medical expenses related to work-related injuries. Through this review process, the necessity and appropriateness of proposed treatment plans are evaluated, ensuring that injured workers receive the proper care to facilitate their recovery while minimizing unnecessary costs.
Fort Collins Colorado Request for Utilization Review for Workers' Compensation
State:
Colorado
City:
Fort Collins
Control #:
CO-WC131R-1-WC
Format:
Word;
PDF;
Rich Text
Instant download
Public form
Description
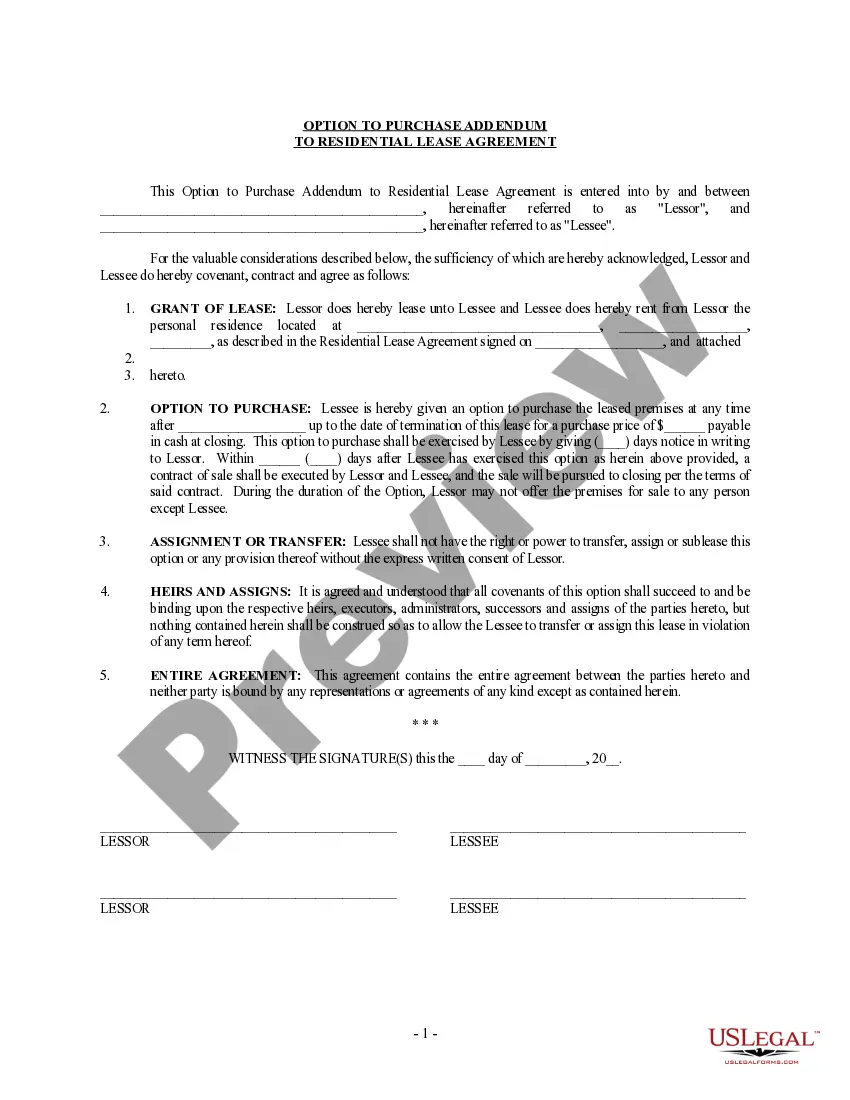
This is one of the official Workers' Compensation forms for the state of Colorado
Fort Collins Colorado Request for Utilization Review for Workers' Compensation is a crucial process that enables employers and insurers to effectively manage and control medical treatment expenses related to work-related injuries. This review ensures that the provided medical care is necessary, appropriate, and aligned with the standards outlined by the Colorado Division of Workers' Compensation. By using relevant keywords, we can provide a detailed description of this process. The Fort Collins Colorado Request for Utilization Review for Workers' Compensation is primarily initiated when an injured worker requires medical treatment following a workplace injury or illness. This request aims to determine the medical necessity and the appropriateness of the proposed treatment plan. Keywords related to this process may include: 1. Utilization Review: The utilization review process involves an assessment of medical treatment plans proposed by healthcare providers to ensure they align with guidelines and standards set forth by the Colorado Division of Workers' Compensation. 2. Workers' Compensation: Workers' compensation refers to a system that provides medical treatment, wage replacement, and other benefits to employees who have been injured or become ill as a result of their job duties. This request is specific to workers' compensation cases in Fort Collins, Colorado. 3. Medical Necessity: Medical necessity refers to the requirement that the proposed treatment or service is appropriate and essential in treating the worker's injury or illness. The utilization review determines if the recommended treatment aligns with this criterion. 4. Treatment Plan: A treatment plan is a comprehensive outline of the medical interventions, therapies, and procedures recommended by the healthcare provider to facilitate the injured worker's recovery. This plan undergoes scrutiny during the utilization review process. Different types of Fort Collins Colorado Requests for Utilization Review for Workers' Compensation may include: 1. Initial Treatment Review: This type of review focuses on the medical treatment plan proposed by the healthcare provider for the immediate management of the worker's injury or illness. 2. Ongoing Treatment Review: As the injured worker's condition progresses, healthcare providers may propose subsequent treatments or therapies. This review assesses the continued necessity and appropriateness of the ongoing treatment plan. 3. Pre-Authorization Review: In some cases, medical treatment may require pre-authorization, especially if it involves certain procedures, surgeries, or medications. This review evaluates whether the requested treatment is essential before approval is granted. 4. Second Opinion Review: Occasionally, a second opinion from another healthcare provider may be sought to validate the initial treatment plan. This review determines the most appropriate course of action based on multiple professional opinions. In conclusion, the Fort Collins Colorado Request for Utilization Review for Workers' Compensation is a critical component of managing and controlling medical expenses related to work-related injuries. Through this review process, the necessity and appropriateness of proposed treatment plans are evaluated, ensuring that injured workers receive the proper care to facilitate their recovery while minimizing unnecessary costs.
How to fill out Fort Collins Colorado Request For Utilization Review For Workers' Compensation?
If you’ve already used our service before, log in to your account and download the Fort Collins Colorado Request for Utilization Review for Workers' Compensation on your device by clicking the Download button. Make certain your subscription is valid. If not, renew it in accordance with your payment plan.
If this is your first experience with our service, follow these simple steps to get your document:
- Make sure you’ve found an appropriate document. Read the description and use the Preview option, if any, to check if it meets your requirements. If it doesn’t suit you, use the Search tab above to get the appropriate one.
- Purchase the template. Click the Buy Now button and choose a monthly or annual subscription plan.
- Register an account and make a payment. Utilize your credit card details or the PayPal option to complete the transaction.
- Get your Fort Collins Colorado Request for Utilization Review for Workers' Compensation. Select the file format for your document and save it to your device.
- Fill out your sample. Print it out or take advantage of professional online editors to fill it out and sign it electronically.
You have constant access to every piece of paperwork you have bought: you can locate it in your profile within the My Forms menu anytime you need to reuse it again. Take advantage of the US Legal Forms service to easily locate and save any template for your individual or professional needs!