Title: Syracuse New York Notice Concerning Continuation of Health Care Coverage: A Comprehensive Overview Introduction: The Syracuse New York Notice Concerning Continuation of Health Care Coverage, often referred to as COBRA (Consolidated Omnibus Budget Reconciliation Act), is a vital document that outlines the rights, options, and obligations of employees and their families to continue healthcare benefits after certain qualifying events such as job loss, reduction in work hours, divorce, or death. 1. Components of Syracuse New York Notice Concerning Continuation of Health Care Coverage: This notice provides detailed information on the following key aspects: a. Eligibility: It highlights the criteria employees and their dependents must meet to qualify for continuation of health care coverage, including specific qualifying events and timeframes. b. Coverage Duration: The notice explains the maximum period for which an individual can maintain continued health care coverage, typically 18 or 36 months depending on the qualifying event. c. Premium Payments: This component outlines the responsibility of the individual to pay the premiums for continued coverage, highlighting the timeline, acceptable payment methods, and potential consequences for late or non-payment. d. Coverage Plans: It provides information about the available healthcare options, including the benefits, limits, and costs associated with each plan. This could involve details regarding medical, dental, vision, and other supplementary coverage. e. Notification Process: The notice outlines employer and employee responsibilities for notifying each other about the occurrence of a qualifying event, as well as the process and timeframe for exercising continuation rights. 2. Types of Syracuse New York Notice Concerning Continuation of Health Care Coverage: a. General COBRA Continuation Notice: This notice is typically provided to employees and their dependents upon initial enrollment in a group health plan, and contains comprehensive information about rights and responsibilities for continued coverage. b. Qualifying Event-Specific Notices: These notices are triggered by specific events such as job loss, divorce, or death and provide affected individuals with the necessary information to exercise their continuation rights based on their circumstances. c. Alternative Coverage Notices: In some cases, an employer may offer alternative coverage options rather than COBRA continuation, such as state-sponsored health insurance programs. Syracuse New York Notice Concerning Continuation of Health Care Coverage may include information about such alternatives, eligibility criteria, and enrollment instructions. Conclusion: The Syracuse New York Notice Concerning Continuation of Health Care Coverage serves as a crucial resource for employees and their dependents to navigate the complex landscape of healthcare coverage after experiencing a qualifying event. Understanding the detailed information within this notice is vital in order to make informed decisions about continuation of health care benefits, ensuring the well-being and financial security of the affected individuals and their families.
Syracuse New York Notice Concerning Continuation of Health Care Coverage
State:
New York
City:
Syracuse
Control #:
NY-807D
Format:
PDF
Instant download
Public form
Description
This form is a notice concerning continuation of health care coverage after a divorce.
Title: Syracuse New York Notice Concerning Continuation of Health Care Coverage: A Comprehensive Overview Introduction: The Syracuse New York Notice Concerning Continuation of Health Care Coverage, often referred to as COBRA (Consolidated Omnibus Budget Reconciliation Act), is a vital document that outlines the rights, options, and obligations of employees and their families to continue healthcare benefits after certain qualifying events such as job loss, reduction in work hours, divorce, or death. 1. Components of Syracuse New York Notice Concerning Continuation of Health Care Coverage: This notice provides detailed information on the following key aspects: a. Eligibility: It highlights the criteria employees and their dependents must meet to qualify for continuation of health care coverage, including specific qualifying events and timeframes. b. Coverage Duration: The notice explains the maximum period for which an individual can maintain continued health care coverage, typically 18 or 36 months depending on the qualifying event. c. Premium Payments: This component outlines the responsibility of the individual to pay the premiums for continued coverage, highlighting the timeline, acceptable payment methods, and potential consequences for late or non-payment. d. Coverage Plans: It provides information about the available healthcare options, including the benefits, limits, and costs associated with each plan. This could involve details regarding medical, dental, vision, and other supplementary coverage. e. Notification Process: The notice outlines employer and employee responsibilities for notifying each other about the occurrence of a qualifying event, as well as the process and timeframe for exercising continuation rights. 2. Types of Syracuse New York Notice Concerning Continuation of Health Care Coverage: a. General COBRA Continuation Notice: This notice is typically provided to employees and their dependents upon initial enrollment in a group health plan, and contains comprehensive information about rights and responsibilities for continued coverage. b. Qualifying Event-Specific Notices: These notices are triggered by specific events such as job loss, divorce, or death and provide affected individuals with the necessary information to exercise their continuation rights based on their circumstances. c. Alternative Coverage Notices: In some cases, an employer may offer alternative coverage options rather than COBRA continuation, such as state-sponsored health insurance programs. Syracuse New York Notice Concerning Continuation of Health Care Coverage may include information about such alternatives, eligibility criteria, and enrollment instructions. Conclusion: The Syracuse New York Notice Concerning Continuation of Health Care Coverage serves as a crucial resource for employees and their dependents to navigate the complex landscape of healthcare coverage after experiencing a qualifying event. Understanding the detailed information within this notice is vital in order to make informed decisions about continuation of health care benefits, ensuring the well-being and financial security of the affected individuals and their families.
How to fill out Syracuse New York Notice Concerning Continuation Of Health Care Coverage?
If you’ve already utilized our service before, log in to your account and save the Syracuse New York Notice Concerning Continuation of Health Care Coverage on your device by clicking the Download button. Make certain your subscription is valid. If not, renew it according to your payment plan.
If this is your first experience with our service, follow these simple actions to get your document:
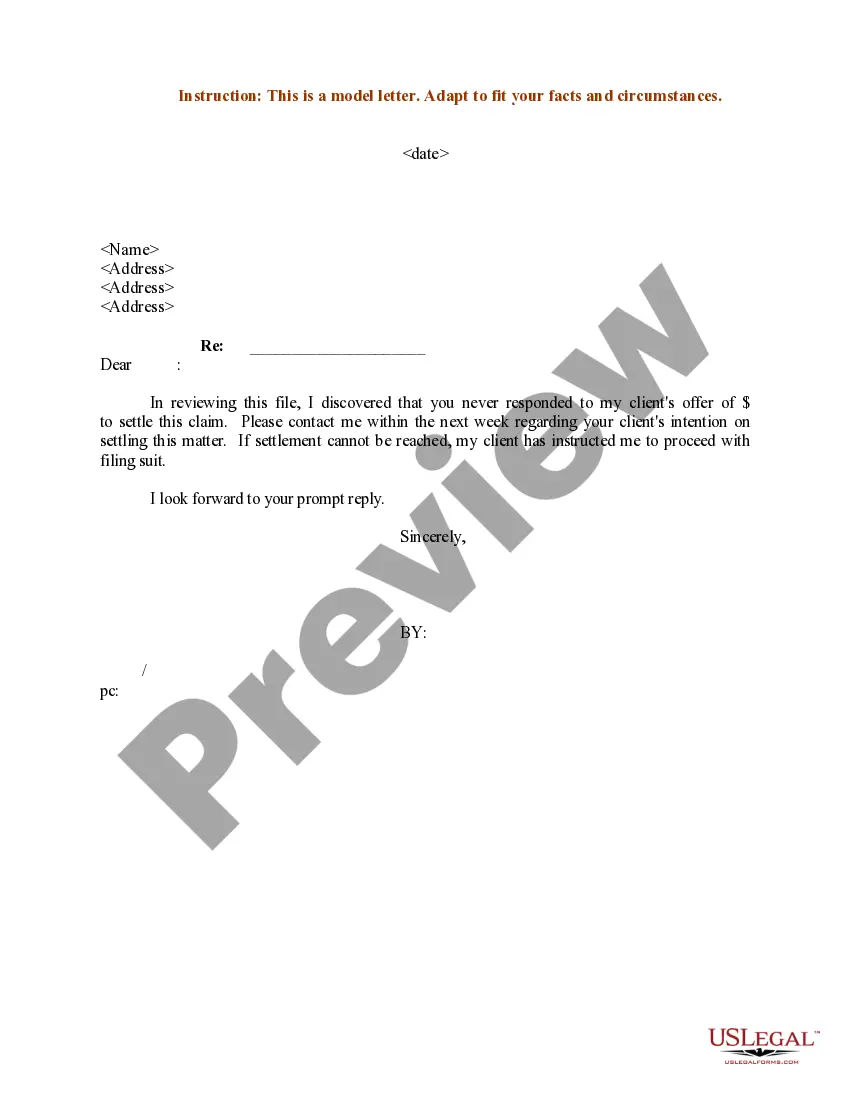
- Ensure you’ve located an appropriate document. Look through the description and use the Preview option, if available, to check if it meets your requirements. If it doesn’t fit you, utilize the Search tab above to find the proper one.
- Purchase the template. Click the Buy Now button and pick a monthly or annual subscription plan.
- Register an account and make a payment. Utilize your credit card details or the PayPal option to complete the purchase.
- Get your Syracuse New York Notice Concerning Continuation of Health Care Coverage. Select the file format for your document and save it to your device.
- Complete your sample. Print it out or take advantage of professional online editors to fill it out and sign it electronically.
You have permanent access to each piece of paperwork you have purchased: you can find it in your profile within the My Forms menu whenever you need to reuse it again. Take advantage of the US Legal Forms service to rapidly find and save any template for your personal or professional needs!