Portland Oregon Complaint for Recovery of Medical Assistance: A Detailed Description Keywords: Portland Oregon, Complaint, Recovery of Medical Assistance, Medical Assistance, Medicaid, Financial Recovery, Overpayments, Fraudulent Claims, Legal Action Introduction: The Portland Oregon Complaint for Recovery of Medical Assistance refers to legal actions initiated by the Oregon Health Authority (OHA) to recover medical assistance funds, commonly known as Medicaid, that have been improperly disbursed or paid as a result of fraudulent claims, overpayments, or other related situations. This complaint serves as a means to reclaim public funds and ensure the integrity and financial sustainability of the Medicaid program in Portland, Oregon. Types of Portland Oregon Complaints for Recovery of Medical Assistance: 1. Medicaid Overpayment Complaint: This type of complaint is filed when the Oregon Health Authority identifies that a healthcare provider has received an excess payment for services provided to Medicaid recipients. Overpayments can occur due to incorrect billing, billing for services not rendered, submission of fraudulent claims, or other discrepancies. The Complaint for Recovery of Medical Assistance seeks restitution of the overpaid amount to protect the financial integrity of the Medicaid program. 2. Fraudulent Claims Complaint: This complaint is filed when there is substantial evidence indicating that a healthcare provider has intentionally submitted false claims for Medicaid reimbursement. These false claims may involve fraudulent billing practices, overcharging, billing for services never performed, or fictitious patient treatment records. The Complaint for Recovery of Medical Assistance aims to recover the ill-gotten funds and deter future fraudulent activities within the Medicaid system. 3. Patient Eligibility Violation Complaint: In certain cases, the OHA may identify instances where Medicaid benefits have been provided to individuals who were not eligible for such assistance. These violations may occur due to intentional misrepresentations by applicants, failure to disclose significant changes in circumstances, or inaccurate eligibility determinations. The Complaint for Recovery of Medical Assistance helps to rectify the financial impact resulting from these eligibility violations and protect the integrity of the Medicaid program. 4. Provider Misconduct Complaint: When healthcare providers engage in unethical or illegal conduct related to the provision of medical services to Medicaid recipients, the OHA may file a Complaint for Recovery of Medical Assistance. This type of complaint seeks to recover funds disbursed to the provider, who may have fraudulently obtained additional reimbursements, disregarded professional standards, or violated specific Medicaid program rules and regulations. Conclusion: The Portland Oregon Complaint for Recovery of Medical Assistance encompasses various types of legal actions taken by the Oregon Health Authority to recover Medicaid funds that have been improperly disbursed or obtained. Whether it involves overpayments, fraudulent claims, patient eligibility violations, or provider misconduct, these complaints are integral in safeguarding the financial viability and sustainability of the Medicaid program in Portland, Oregon. By taking appropriate legal actions, the OHA aims to deter fraud, recover allocated funds, and ensure that the Medicaid program continues to provide vital healthcare assistance to those who truly need it.
Portland Oregon Complaint for Recovery of Medical Assistance
Description
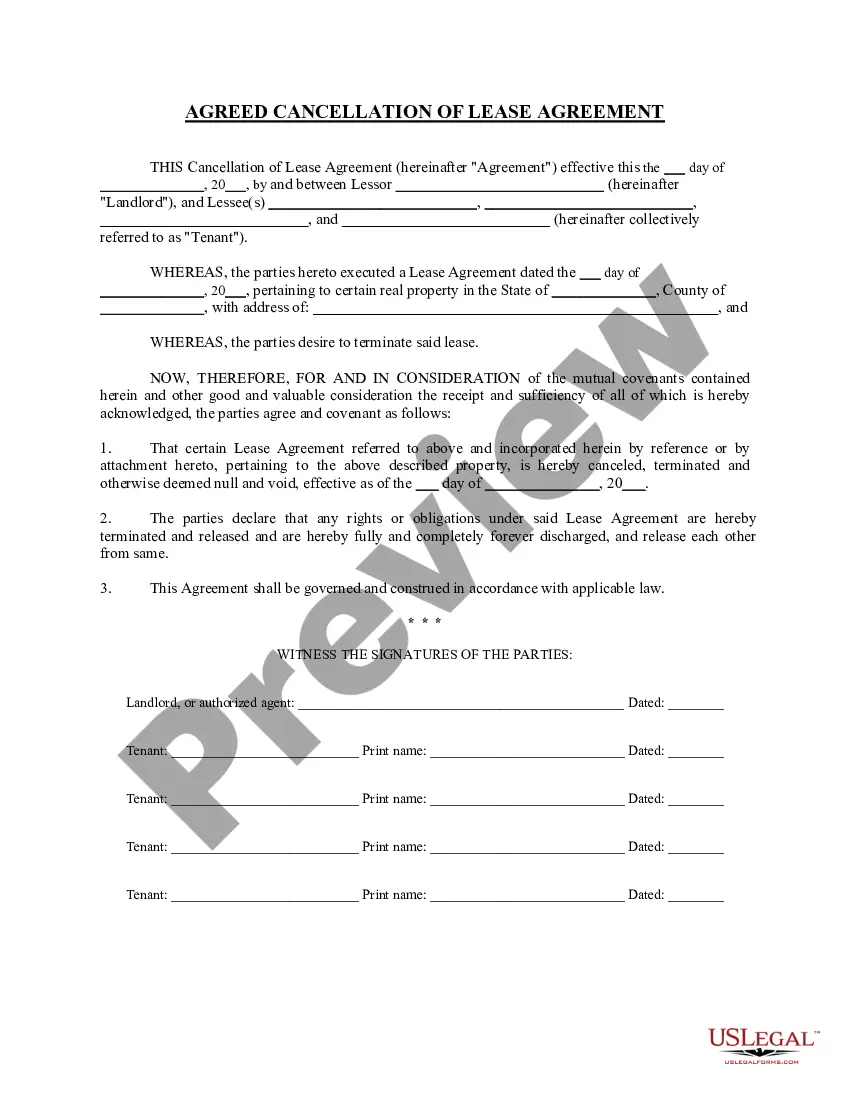
How to fill out Portland Oregon Complaint For Recovery Of Medical Assistance?
If you are looking for a legitimate form template, it’s challenging to locate a more user-friendly service than the US Legal Forms site – likely the most extensive libraries on the web.
Here you can obtain countless form samples for business and personal needs categorized by types and states, or keywords.
With the top-notch search feature, finding the latest Portland Oregon Complaint for Recovery of Medical Assistance is as straightforward as 1-2-3.
Complete the payment. Use your credit card or PayPal account to finalize the registration process.
Acquire the template. Select the file format and save it to your device.
- Additionally, the validity of each document is confirmed by a team of professional attorneys who routinely review the templates on our platform and refresh them according to the most recent state and county requirements.
- If you are already familiar with our system and have a registered account, all you need to do to access the Portland Oregon Complaint for Recovery of Medical Assistance is to Log In to your user account and click the Download option.
- If you are using US Legal Forms for the first time, just follow the instructions listed below.
- Ensure you have located the form you need. Review its details and use the Preview option (if available) to verify its content. If it doesn’t fulfill your needs, use the Search field at the top of the page to find the necessary document.
- Verify your choice. Select the Buy now option. After that, choose the desired subscription plan and provide the details to register for an account.
Form popularity
FAQ
File a complaint with your local consumer protection office or the state agency that regulates the company. Notify the Better Business Bureau (BBB) in your area about your problem. The BBB tries to resolve your complaints against companies.
10 Effective Ways to Complain About a Company Online Go to the company website.Contact the Better Business Bureau.Contact the Federal Trade Commission (FTC).Check out the Ripoff Report.Email spam@uce.gov.Try Yelp.Post on Planet Feedback.Google your attorney general.
The FTC cannot resolve individual complaints, but it can provide information about what steps to take. The FTC says that complaints can help it and its law enforcement partners detect patterns of fraud and abuse, which may lead to investigations and stopping unfair business practices.
Once a complaint is filed, the consumer court investigates the claim. In some cases, they can even suspend the concerned doctor's license if he or she is found responsible for gross negligence. The victim can instead choose to approach a Patient-Advocate, who is someone who conveys medical duty owed to the patient.
You may file a Security Rule complaint electronically via the OCR Complaint Portal, or using our Health Information Privacy Complaint Package - PDF. If you mail or fax the complaint, be sure to send it to the appropriate OCR regional office based on where the alleged violation took place.
10 common customer complaints Product is out of stock.Broken/defective product.Product doesn't meet expectations.Preferred payment not accepted.Long hold times.Disinterested customer service.Having to restate the issue.Issue not resolved on first call.
OHP Member Appeals They can appeal the decision with their CCO or dental plan. After the appeal they can also ask OHA for a hearing. See the OHP Rules (410-141-3875 through 3915) for more about appeals. See the OHP General Rules (410-120-1860) for more about hearings.
If you see a possible violation of the law, you can report it to the Oregon Public Health Division for investigation and further action. Use the online complaint form below or call 1-866-621-6107.
APPLICATION PROCEDURE To file a complaint, write a letter or send a completed complaint form to the Office of the Attorney General, Public Inquiry Unit at the mailing address above. Consumer complaint forms can also be submitted online at: .
Submit the complaint in person or via mail to: Health License Office, 1430 Tandem Ave. NE, Suite 180, Salem, OR 97301, fax: (503) 370-9216, or email: hlo.info@dhsoha.state.or.us.