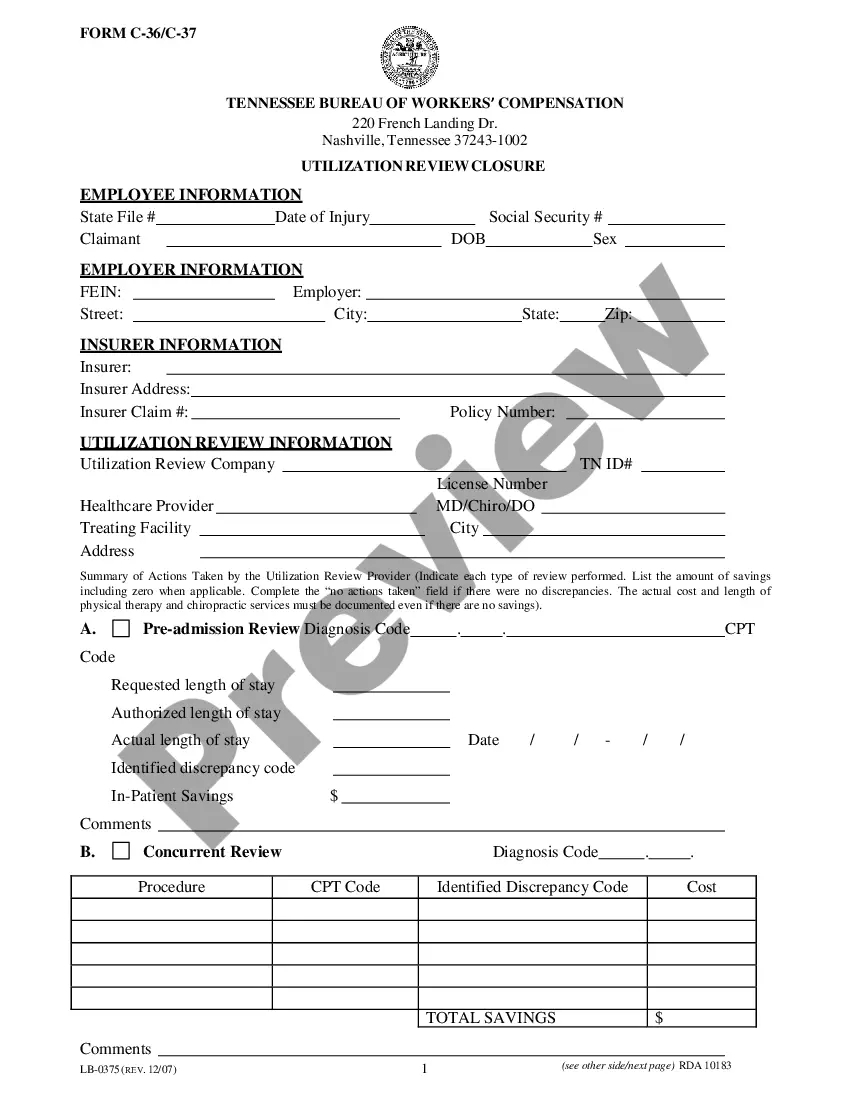
Official Workers' Compensation form in pdf format.
Memphis Tennessee Utilization Review Notification for Workers' Compensation is a process implemented by the state of Tennessee to ensure efficient use of medical resources and appropriate medical treatment for workers who have experienced work-related injuries or illnesses. In this context, "utilization review" refers to the evaluation and assessment of medical services, treatments, and hospital visits to determine their necessity and reasonableness in treating workers' compensate conditions. This process helps to control costs, minimize unnecessary medical procedures, and ensure that injured workers receive proper care, thereby promoting their recovery and a timely return to work. The utilization review notification in Memphis, Tennessee, involves the communication between healthcare providers and employers or workers' compensation insurance carriers regarding the proposed medical treatment. When a healthcare provider proposes a significant medical treatment or service, they must send a notification to the employer or insurance carrier. This notice typically outlines the details of the proposed treatment, including the diagnosis, recommended procedure, expected cost, and expected duration of treatment. Several types of Memphis Tennessee Utilization Review Notifications for Workers' Compensation may exist, depending on the specific circumstances and details of the proposed medical treatment. These variations may include: 1. Initial Treatment Plan Notification: This type of notification is sent when a healthcare provider proposes the initial course of medical treatment for the compensation injury or illness. It usually includes details about the recommended diagnostic tests, medication, therapy, or surgical procedures. 2. Reauthorization Notification: If a worker's medical treatment requires ongoing care, such as physical therapy sessions or prescription medication refills, additional notifications may be necessary whenever reauthorization is required. This ensures that continued treatment is appropriate and justified. 3. Specialist Consultation Notification: When a treating physician recommends the involvement of a specialist for further evaluation or treatment, a specialist consultation notification may be sent. It informs the employer or insurance carrier about the need for an additional medical expert's opinion or services. 4. Surgery Notification: In case a surgical procedure is recommended, a surgery notification is submitted to inform the employer or insurance carrier of the proposed surgical intervention. It includes surgical details, such as the reason for surgery, the type of procedure, and the expected surgical date. By implementing the Memphis Tennessee Utilization Review Notification for Workers' Compensation, the state aims to ensure that workers receive appropriate and effective medical care, reduce unnecessary costs, and facilitate prompt recovery and return to work. This process promotes a fair and efficient workers' compensation system that benefits both employees and employers by optimizing healthcare resources and outcomes.