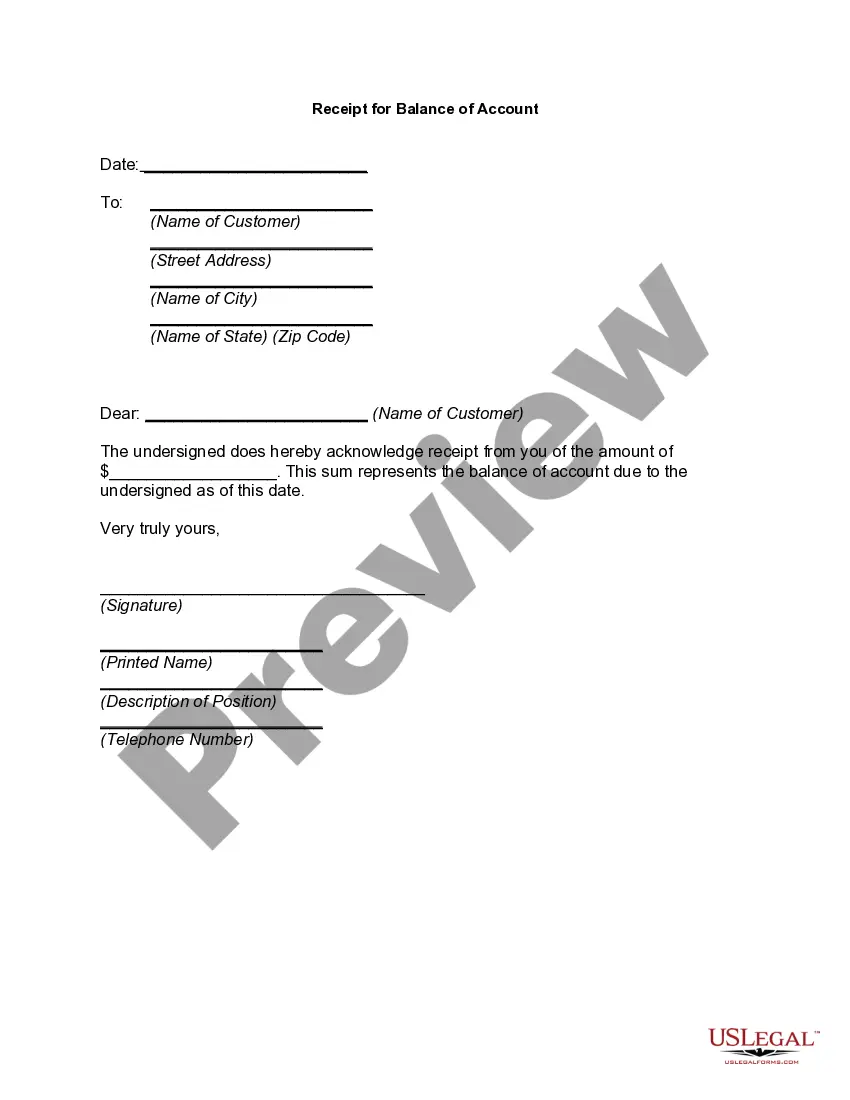
Official Workers' Compensation form in pdf format.
Chattanooga Tennessee Utilization Review Closure for Workers' Compensation refers to the process that occurs when a utilization review decision is made in relation to a workers' compensation claim in Chattanooga, Tennessee. This closure involves a thorough evaluation and decision on the medical treatment or services requested by an injured employee in order to determine if it meets the necessary criteria for approval. The utilization review process in Chattanooga, Tennessee involves various steps to ensure appropriate medical care and cost containment for workers' compensation claims. In some cases, multiple types of closures may arise during this process. Let's explore these closures along with their respective descriptions and keywords: 1. Full Approval Closure: In this type of closure, the utilization review determines that the requested medical treatment or services fully meet the necessary criteria established by the workers' compensation guidelines. The closure indicates that the requested treatment is authorized, and the injured worker can proceed with receiving the prescribed medical care. Keywords: Chattanooga utilization review closure, workers' compensation full approval, approved treatment, authorized medical services. 2. Partial Approval Closure: In instances where the utilization review finds that some aspects of the requested medical treatment or services meet the necessary criteria, but others do not, a partial approval closure occurs. This closure indicates that certain elements of the requested treatment are authorized while others require additional review or modification. Keywords: Partial approval closure, Chattanooga utilization review, workers' compensation, partially approved treatment, authorized services with modifications. 3. Denial Closure: Denial closure arises when the utilization review determines that the requested medical treatment or services do not meet the criteria established by the workers' compensation guidelines. This closure states that the treatment is not authorized, and the injured worker will not receive coverage for the requested services. Keywords: Chattanooga utilization review denial, workers' compensation denial closure, denied treatment, unauthorized medical services. 4. Deferred Closure: In some cases, the utilization review may require additional information or documentation to make a final determination. A deferred closure indicates that the review process has been temporarily put on hold until the necessary data is provided. Keywords: Deferred utilization review closure, Chattanooga workers' compensation, review pending, additional documentation required. The Chattanooga Tennessee Utilization Review Closure for Workers' Compensation is a critical step in ensuring appropriate medical care while containing costs within the workers' compensation system. It aims to strike a balance between the interests of injured employees and the employers' responsibility for providing adequate coverage.Chattanooga Tennessee Utilization Review Closure for Workers' Compensation refers to the process that occurs when a utilization review decision is made in relation to a workers' compensation claim in Chattanooga, Tennessee. This closure involves a thorough evaluation and decision on the medical treatment or services requested by an injured employee in order to determine if it meets the necessary criteria for approval. The utilization review process in Chattanooga, Tennessee involves various steps to ensure appropriate medical care and cost containment for workers' compensation claims. In some cases, multiple types of closures may arise during this process. Let's explore these closures along with their respective descriptions and keywords: 1. Full Approval Closure: In this type of closure, the utilization review determines that the requested medical treatment or services fully meet the necessary criteria established by the workers' compensation guidelines. The closure indicates that the requested treatment is authorized, and the injured worker can proceed with receiving the prescribed medical care. Keywords: Chattanooga utilization review closure, workers' compensation full approval, approved treatment, authorized medical services. 2. Partial Approval Closure: In instances where the utilization review finds that some aspects of the requested medical treatment or services meet the necessary criteria, but others do not, a partial approval closure occurs. This closure indicates that certain elements of the requested treatment are authorized while others require additional review or modification. Keywords: Partial approval closure, Chattanooga utilization review, workers' compensation, partially approved treatment, authorized services with modifications. 3. Denial Closure: Denial closure arises when the utilization review determines that the requested medical treatment or services do not meet the criteria established by the workers' compensation guidelines. This closure states that the treatment is not authorized, and the injured worker will not receive coverage for the requested services. Keywords: Chattanooga utilization review denial, workers' compensation denial closure, denied treatment, unauthorized medical services. 4. Deferred Closure: In some cases, the utilization review may require additional information or documentation to make a final determination. A deferred closure indicates that the review process has been temporarily put on hold until the necessary data is provided. Keywords: Deferred utilization review closure, Chattanooga workers' compensation, review pending, additional documentation required. The Chattanooga Tennessee Utilization Review Closure for Workers' Compensation is a critical step in ensuring appropriate medical care while containing costs within the workers' compensation system. It aims to strike a balance between the interests of injured employees and the employers' responsibility for providing adequate coverage.