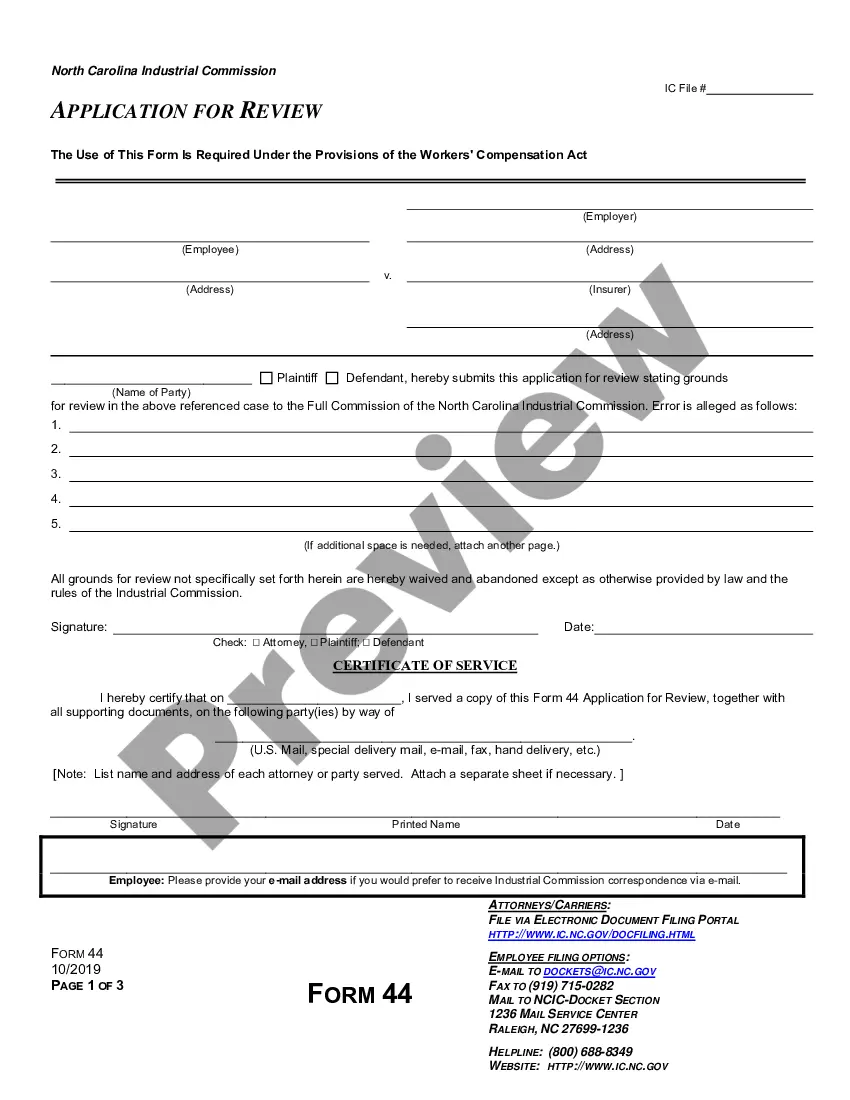
Official Workers' Compensation form in pdf format.
Clarksville Tennessee Utilization Review Closure for Workers' Compensation is a process that refers to the evaluation and termination of workers' compensation claims in the Clarksville, Tennessee area. This process involves reviewing and assessing the necessity and appropriateness of medical treatments and services rendered to injured workers. By implementing utilization review closure, employers and insurers aim to control costs, ensure fair and valid claims, and facilitate the return-to-work process for employees. Keywords: Clarksville Tennessee, Utilization Review Closure, Workers' Compensation, claims, evaluation, termination, medical treatments, services, injured workers, employers, insurers, control costs, fair claims, valid claims, return-to-work process. Types of Clarksville Tennessee Utilization Review Closure for Workers' Compensation: 1. Medical Necessity Review: This type of closure focuses on assessing the medical treatments and services provided to injured workers and determining their necessity. Medical professionals review the treatments to ensure they are appropriate, effective, and aligned with evidence-based medicine guidelines. 2. Preauthorization Review: Utilization review closure may involve a preauthorization process, where medical treatments and services are evaluated before they are provided. This type of closure ensures that only essential and reasonable treatments are authorized in a workers' compensation claim. 3. Claim File Review: In this type of closure, the entire workers' compensation claim file is reviewed comprehensively. This includes examining medical records, treatment plans, progress notes, and other relevant documentation to determine if the claim is legitimate and if further treatments are required. 4. Independent Medical Examination (IME): Utilization review closure may also involve an independent medical examination. Times are typically conducted by a qualified and impartial medical professional who reviews the injured worker's medical history, conducts a physical examination, and offers an expert opinion on the necessity and extent of ongoing treatments. 5. Cost Containment Review: This type of closure focuses on controlling costs associated with workers' compensation claims. It involves assessing the medical treatments and services for potential cost-saving opportunities without compromising the injured worker's well-being. In summary, Clarksville Tennessee Utilization Review Closure for Workers' Compensation is a vital part of the claims' management process. It involves various types of reviews, including medical necessity, preauthorization, claim file, independent medical examination, and cost containment reviews. These reviews aim to ensure that injured workers receive appropriate and necessary medical treatments while controlling costs and facilitating their return to work.