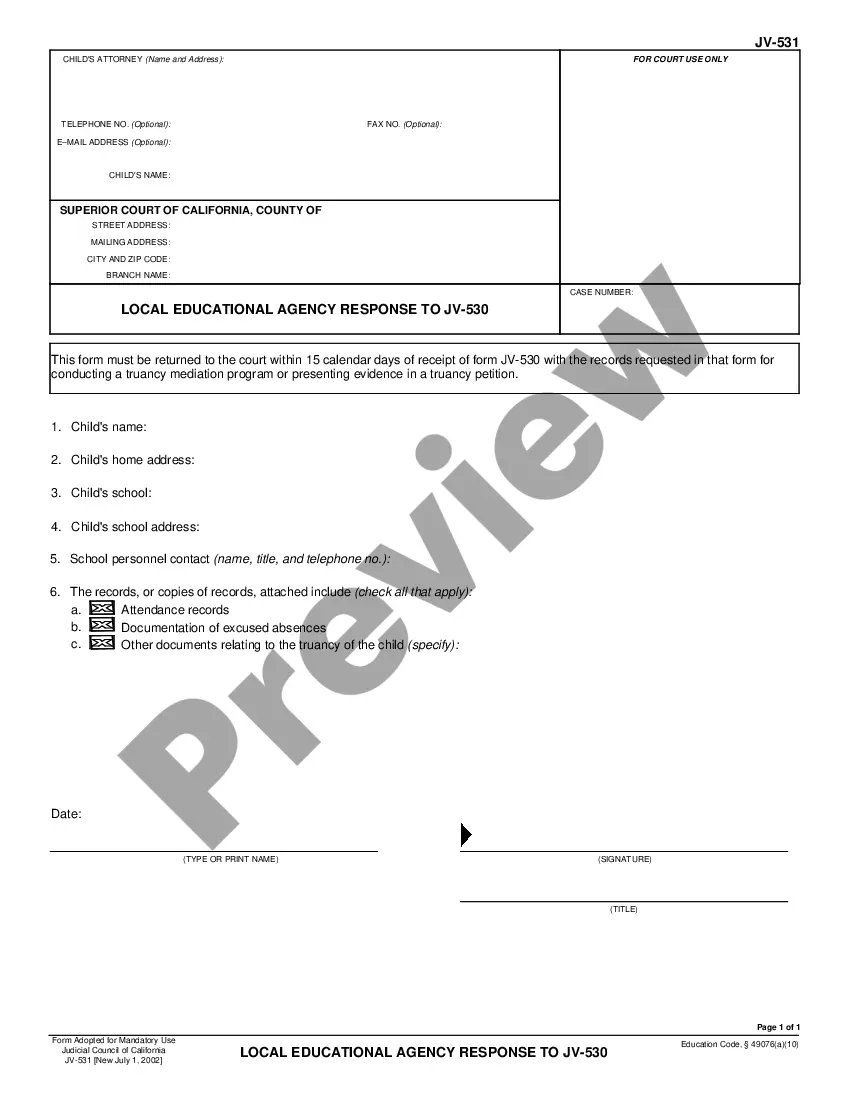
Official Workers' Compensation form in pdf format.
Memphis Tennessee Utilization Review Closure for Workers' Compensation involves the process of evaluating and determining the appropriateness and necessity of medical treatments and services provided to injured workers under the workers' compensation system in the state of Tennessee, specifically in the city of Memphis. Utilization review is a crucial step in ensuring that injured workers receive appropriate and evidence-based medical care while minimizing unnecessary expenses and avoiding over utilization of medical services. It aims to strike a balance between the injured worker's needs for timely and effective medical treatment and the employer's/insurer's responsibility to contain costs and promote efficient care. The utilization review closure entails the evaluation and assessment of medical records, treatment plans, and other relevant information pertaining to the injured worker's condition. Trained professionals, such as utilization review nurses and physicians, carefully review the provided information to determine if the medical treatment and services align with the established guidelines, standards, and protocols. The closure process helps ensure that the injured worker received all necessary and appropriate care required for their recovery. If the utilization review determines that the treatment plan and services have been satisfactorily completed, closure is indicated. On the other hand, if the review identifies any issues or potential discrepancies, it may require further investigation, adjustments, or additional interventions to ensure the injured worker's well-being. There may be different types of utilization review closure for workers' compensation in Memphis, Tennessee, which vary based on the specific circumstances and requirements of the case. These may include: 1. Medical Treatment Closure: This type of closure occurs when the utilization review determines that the injured worker has received sufficient medical treatment to address their work-related injury or illness adequately. It signifies that the injured worker has reached a point of maximum medical improvement, where further treatment is unlikely to result in significant additional improvement. 2. Claim Closure: In some cases, the utilization review closure may coincide with the closure of the workers' compensation claim itself. This closure typically occurs when the injured worker has fully recovered from their work-related injury or illness and no longer requires any further medical treatment or benefits. 3. Utilization Review Appeal Closure: Occasionally, the utilization review process may involve an appeal if there are disagreements or disputes regarding the initial decision. Utilization review appeal closure signifies the final decision reached after the appeal process, confirming the appropriateness or denial of the requested medical treatment and services. It is important to note that the specific types of utilization review closure may vary depending on the workers' compensation laws and regulations in Memphis, Tennessee. The primary goal of all these closure types is to ensure the injured worker receives proper care and that the employer/insurer fulfills their obligations while maintaining cost control and efficient utilization of resources.Memphis Tennessee Utilization Review Closure for Workers' Compensation involves the process of evaluating and determining the appropriateness and necessity of medical treatments and services provided to injured workers under the workers' compensation system in the state of Tennessee, specifically in the city of Memphis. Utilization review is a crucial step in ensuring that injured workers receive appropriate and evidence-based medical care while minimizing unnecessary expenses and avoiding over utilization of medical services. It aims to strike a balance between the injured worker's needs for timely and effective medical treatment and the employer's/insurer's responsibility to contain costs and promote efficient care. The utilization review closure entails the evaluation and assessment of medical records, treatment plans, and other relevant information pertaining to the injured worker's condition. Trained professionals, such as utilization review nurses and physicians, carefully review the provided information to determine if the medical treatment and services align with the established guidelines, standards, and protocols. The closure process helps ensure that the injured worker received all necessary and appropriate care required for their recovery. If the utilization review determines that the treatment plan and services have been satisfactorily completed, closure is indicated. On the other hand, if the review identifies any issues or potential discrepancies, it may require further investigation, adjustments, or additional interventions to ensure the injured worker's well-being. There may be different types of utilization review closure for workers' compensation in Memphis, Tennessee, which vary based on the specific circumstances and requirements of the case. These may include: 1. Medical Treatment Closure: This type of closure occurs when the utilization review determines that the injured worker has received sufficient medical treatment to address their work-related injury or illness adequately. It signifies that the injured worker has reached a point of maximum medical improvement, where further treatment is unlikely to result in significant additional improvement. 2. Claim Closure: In some cases, the utilization review closure may coincide with the closure of the workers' compensation claim itself. This closure typically occurs when the injured worker has fully recovered from their work-related injury or illness and no longer requires any further medical treatment or benefits. 3. Utilization Review Appeal Closure: Occasionally, the utilization review process may involve an appeal if there are disagreements or disputes regarding the initial decision. Utilization review appeal closure signifies the final decision reached after the appeal process, confirming the appropriateness or denial of the requested medical treatment and services. It is important to note that the specific types of utilization review closure may vary depending on the workers' compensation laws and regulations in Memphis, Tennessee. The primary goal of all these closure types is to ensure the injured worker receives proper care and that the employer/insurer fulfills their obligations while maintaining cost control and efficient utilization of resources.