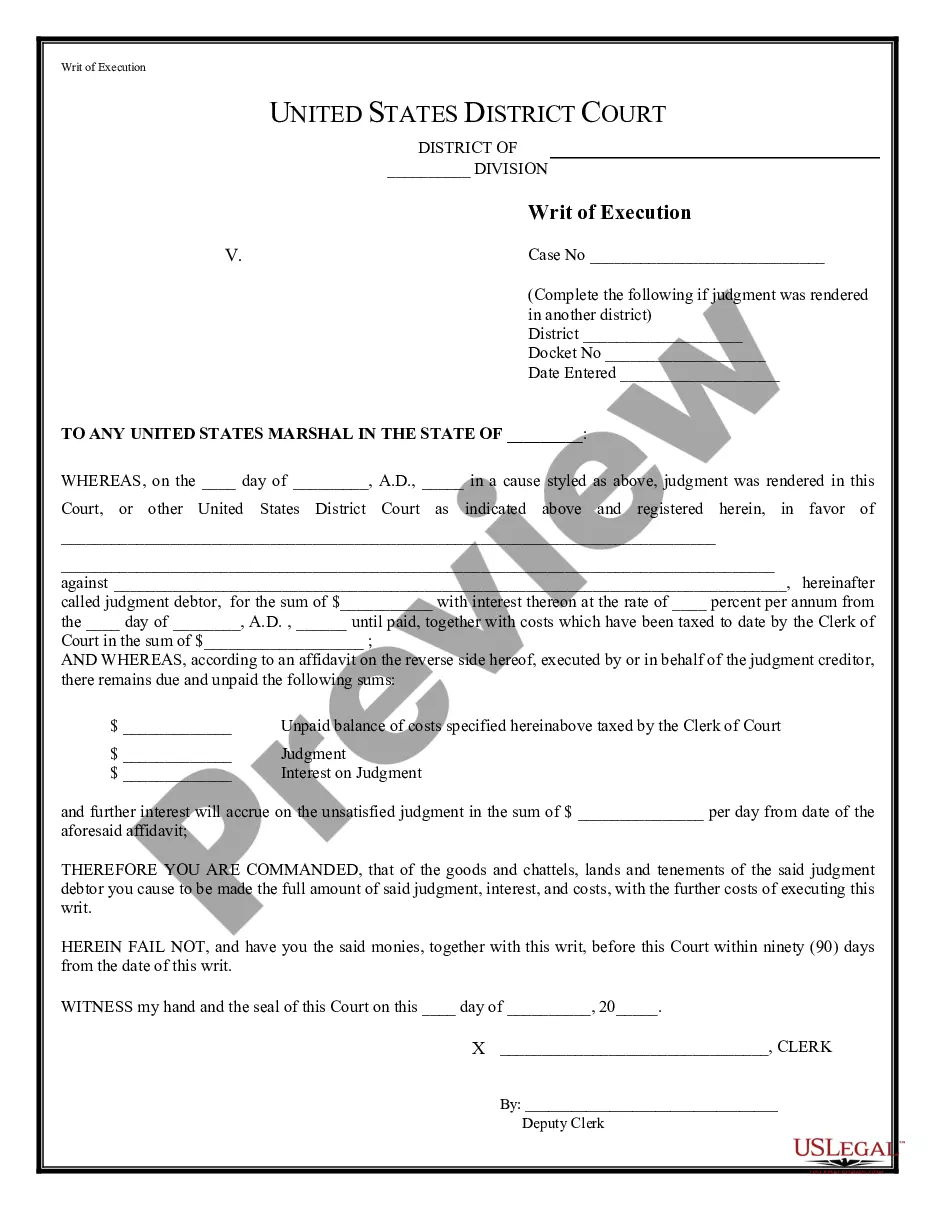
Official Workers' Compensation form in pdf format.
Murfreesboro Tennessee Utilization Review Closure for Workers' Compensation is a necessary process that ensures the proper management of workers' compensation claims in Murfreesboro, Tennessee. It involves a comprehensive review of medical treatment plans and services provided to injured workers by healthcare providers, with a focus on ensuring their appropriateness, effectiveness, and efficiency. The primary goal of the utilization review closure is to streamline the claims process while safeguarding the interests of both injured workers and insurance providers. By carefully analyzing medical records, treatment plans, and related documentation, the closure process aims to determine the necessity and quality of medical care received by injured employees. The Murfreesboro Tennessee Utilization Review Closure for Workers' Compensation can be categorized into various types based on different aspects. These include: 1. Medical Necessity Review: This type of review carefully evaluates whether the medical treatment received by the injured worker was necessary for their recovery and overall well-being. It assesses the appropriateness of the treatment plan and identifies any excessive or unnecessary procedures or services. 2. Treatment Efficacy Review: This review focuses on gauging the effectiveness of the medical treatment provided. It analyzes the outcomes of the treatment, including the progress made by the injured worker, improvement in their condition, and whether the treatment met the expected goals. 3. Cost Containment Review: This type of review primarily concentrates on controlling the costs associated with workers' compensation claims. It aims to identify any excessive billing, over utilization of medical services, or unnecessary expenses, ensuring that only the required medical services are authorized for payment. 4. Medical Peer Review: This review involves an in-depth analysis of the medical records and treatment plans by qualified medical professionals. They assess whether the treatment was in line with generally accepted medical guidelines and standards, providing an expert opinion on the appropriateness and quality of care received. The Murfreesboro Tennessee Utilization Review Closure for Workers' Compensation is critical in protecting both the rights and well-being of injured employees, as well as the financial stability of insurance providers. Through a diligent review process, it helps ensure that appropriate medical care is provided, facilitating the efficient resolution of workers' compensation claims.