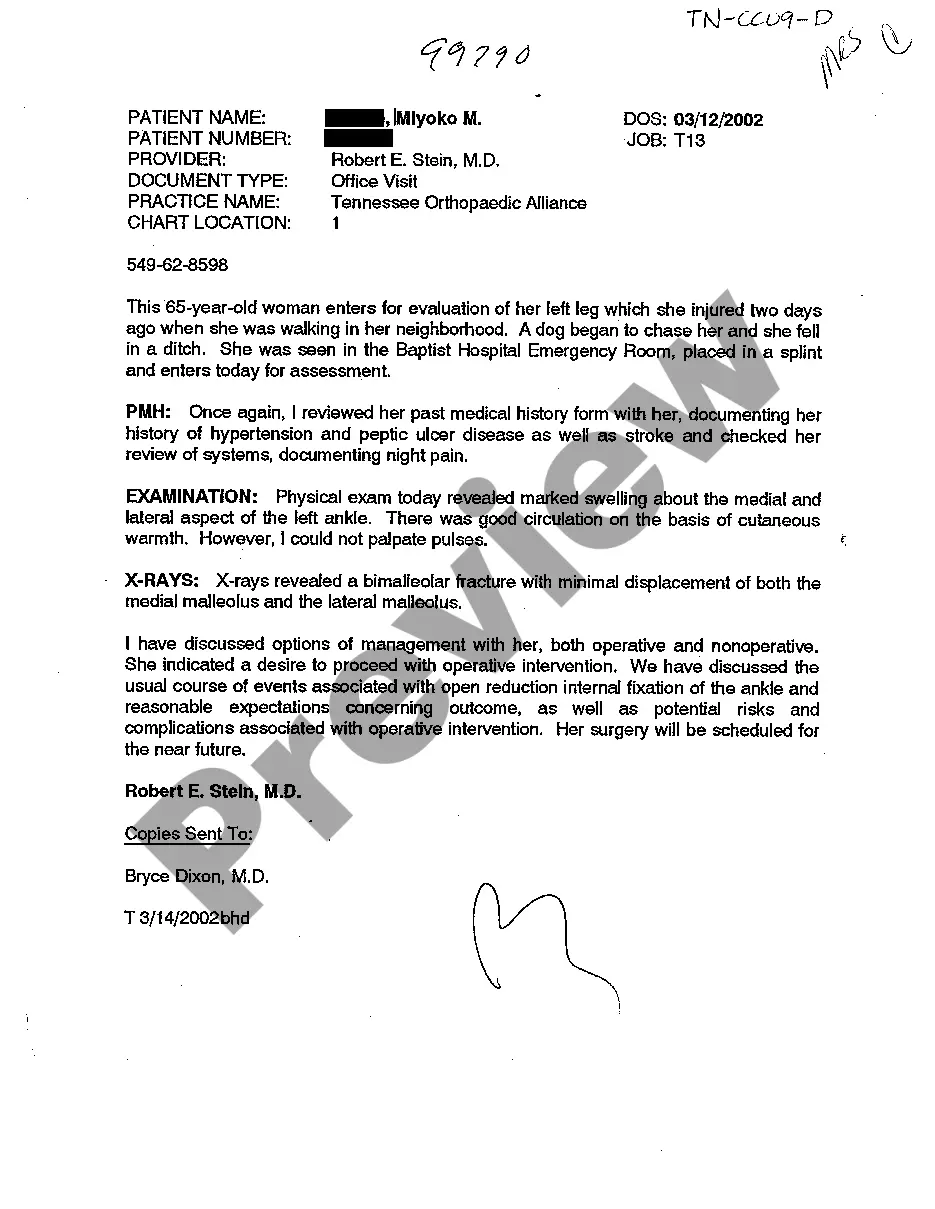
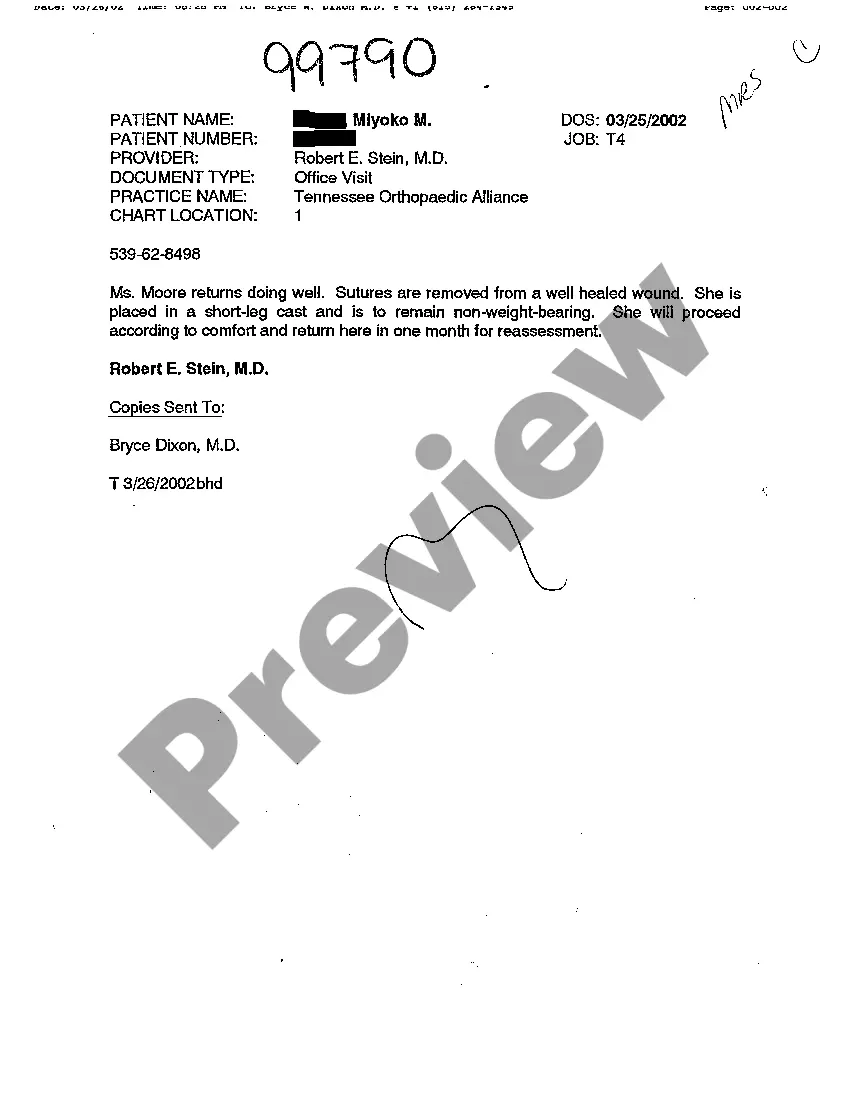
Chattanooga, Tennessee Examination Notes of Treating Physician play a crucial role in the medical field by documenting patient visits, diagnoses, treatments, and other important medical information. These notes serve as a vital resource for healthcare providers to track a patient's progress, determine appropriate treatment plans, and ensure continuity of care. The primary purpose of Chattanooga Tennessee Examination Notes of Treating Physician is to accurately record the patient's medical history, symptoms, and physical examination findings. The notes include comprehensive details about the patient's complaints, such as the nature and duration of symptoms, possible triggers, and any relevant medical history or family history. Additionally, the physician's observations, including vital signs, physical examination findings, and assessment of the patient's general health and well-being, are meticulously recorded. In addition to the initial assessment, Chattanooga Tennessee Examination Notes of Treating Physician also document the physician's diagnosis and recommended treatment plan. This includes prescribing medications, recommending further tests or procedures, and providing advice on lifestyle modifications or therapeutic interventions. These notes serve as a reference for future visits, allowing the physician to track the patient's response to treatment or changes in their condition. There are several types of Chattanooga Tennessee Examination Notes of Treating Physician, including: 1. Initial Consultation Notes: These notes detail the patient's first visit to the treating physician, including their presenting symptoms, medical history, physical examination findings, and initial impressions of the diagnosis. This serves as the baseline for future treatment and progress monitoring. 2. Follow-up Examination Notes: These notes capture subsequent visits and record the patient's progress, treatment response, and any adjustments made to the initial treatment plan. They may also include any additional diagnostic tests or referrals performed during these visits. 3. Surgical or Procedural Examination Notes: In cases where the treating physician performs a surgical procedure or medical intervention, detailed examination notes are essential. These notes document preoperative assessments, intraoperative findings, any complications encountered, and postoperative progress. 4. Specialty-Specific Examination Notes: Different medical specialties require tailored examination notes. For example, a cardiologist's notes may focus on the cardiovascular system, including findings from electrocardiograms, echocardiograms, or stress tests. On the other hand, an orthopedic surgeon's notes may focus on musculoskeletal assessments, X-ray findings, or surgical considerations. 5. Mental Health Examination Notes: Psychiatrists, psychologists, or counselors maintain examination notes specifically for mental health evaluations. These notes capture the patient's psychiatric history, mental status examination, diagnostic impressions, treatment plans, and progress monitoring. In summary, Chattanooga Tennessee Examination Notes of Treating Physician are comprehensive and detailed records that document various aspects of a patient's medical journey. They provide vital information for healthcare providers to make well-informed decisions, track patient progress, and ensure effective, personalized treatment plans. Whether it is an initial consultation, a follow-up visit, a surgical case, or a mental health evaluation, these examination notes are essential in providing quality healthcare.
Chattanooga Tennessee Examination Notes of Treating Physician
Description
How to fill out Chattanooga Tennessee Examination Notes Of Treating Physician?
Do you require a reliable and economical provider of legal documents to obtain the Chattanooga Tennessee Examination Notes of Treating Physician? US Legal Forms is your prime choice.
Whether you need a simple agreement to establish rules for living together with your partner or a collection of papers to expedite your divorce through the court, we are here to assist you. Our site features over 85,000 current legal document templates for personal and commercial use.
All templates that we offer access to are not generic and are tailored according to the mandates of specific states and locales.
To acquire the document, you must Log Into your account, locate the required form, and click the Download button adjacent to it. Please remember that you can download your previously purchased form templates at any time from the My documents section.
Now you can create your account. Then choose the subscription plan and proceed to payment.
After the payment is finalized, download the Chattanooga Tennessee Examination Notes of Treating Physician in any available format. You can return to the website at any moment and redownload the document at no additional cost.
- Is this your first time visiting our platform? No need to worry.
- You can set up an account within moments, but first, ensure that you do the following.
- Verify if the Chattanooga Tennessee Examination Notes of Treating Physician complies with the regulations of your state and local jurisdiction.
- Review the form’s specifics (if accessible) to determine who and what the document is meant for.
- If the form does not suit your legal circumstances, start the search again.
Form popularity
FAQ
In Tennessee, a physician can supervise up to three Physician Assistants. This regulation ensures that quality care is maintained while allowing physicians to expand their practice effectively. It is vital for healthcare providers to understand these guidelines as they pertain to their practice. Therefore, topics like Chattanooga Tennessee Examination Notes of Treating Physician become essential for compliance.
Doctors in Tennessee are regulated by the Tennessee Board of Medical Examiners, which oversees licensing and professional conduct. This board ensures that all practicing physicians adhere to state laws and standards. Regular evaluations and feedback help maintain high medical standards. As such, Chattanooga Tennessee Examination Notes of Treating Physician contribute to these regulatory efforts.
The most common medical complaints reported to doctors include issues like pain, fatigue, and anxiety. These complaints often lead patients to seek help to improve their quality of life. Acknowledging and addressing these common concerns is critical for effective treatment. Thus, Chattanooga Tennessee Examination Notes of Treating Physician play an important role in managing these issues.
The most common complaints at the doctor's office often involve miscommunication about treatment plans and prescription refills. Many patients express dissatisfaction with wait times and clarity of instructions given. Understanding these issues fosters better patient-provider relationships and improves overall care experience. Staying informed about such complaints can illuminate aspects of Chattanooga Tennessee Examination Notes of Treating Physician.
To add a supervising physician in Tennessee, you must submit a Supervisory Agreement to the Tennessee Board of Medical Examiners. This document outlines the responsibilities and authority of both the supervising physician and the practitioner. Be sure to include all required details and signatures to ensure compliance with state regulations. This process is especially relevant when discussing Chattanooga Tennessee Examination Notes of Treating Physician.
Filing a complaint against a doctor in Tennessee starts with gathering your information and evidence. You can file a formal complaint using the Board of Medical Examiners' website. It is essential to include all pertinent details about your experience to support your claim. This proactive approach can lead to improvements in practices related to Chattanooga Tennessee Examination Notes of Treating Physician.
To email the Tennessee Board of Medical Examiners, locate the contact information on their official website. You should provide a clear subject line that reflects your inquiry or concern. In your email, be succinct and include your contact information for a prompt response. This is a vital step if you have questions about the Chattanooga Tennessee Examination Notes of Treating Physician.
Reporting a doctor to the medical board in Tennessee involves submitting a formal complaint through the Tennessee Board of Medical Examiners. You can complete an online complaint form available on their website. Ensure that you provide specific details about your concerns, including your experiences and any relevant documentation. Engaging with the process can help improve the standards of care, particularly regarding Chattanooga Tennessee Examination Notes of Treating Physician.
To get your medical records in Tennessee, start by contacting your healthcare provider directly. You will need to submit a request that clearly states what records you want, including any Chattanooga Tennessee Examination Notes of Treating Physician. Many providers now have online portals that facilitate this request process. If you encounter difficulties, consider using uslegalforms to obtain tailored templates and ensure a smooth retrieval of your records.
The easiest way to get medical records often involves using an online platform that specializes in this service. These platforms can simplify the process of requesting your Chattanooga Tennessee Examination Notes of Treating Physician by allowing you to submit requests electronically. They often provide guidelines and ensure that your request meets the necessary legal requirements. This saves you time and reduces the hassle of paperwork.