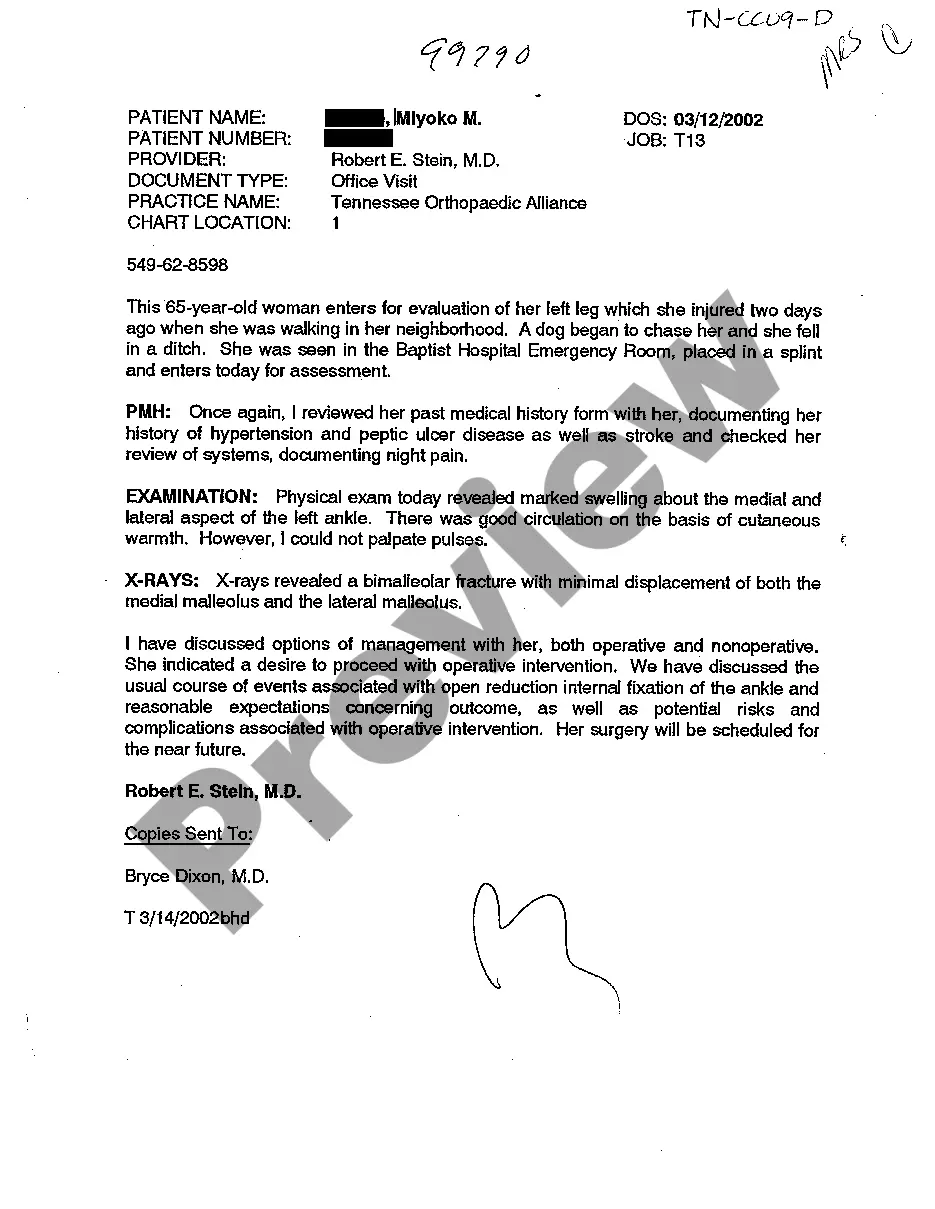
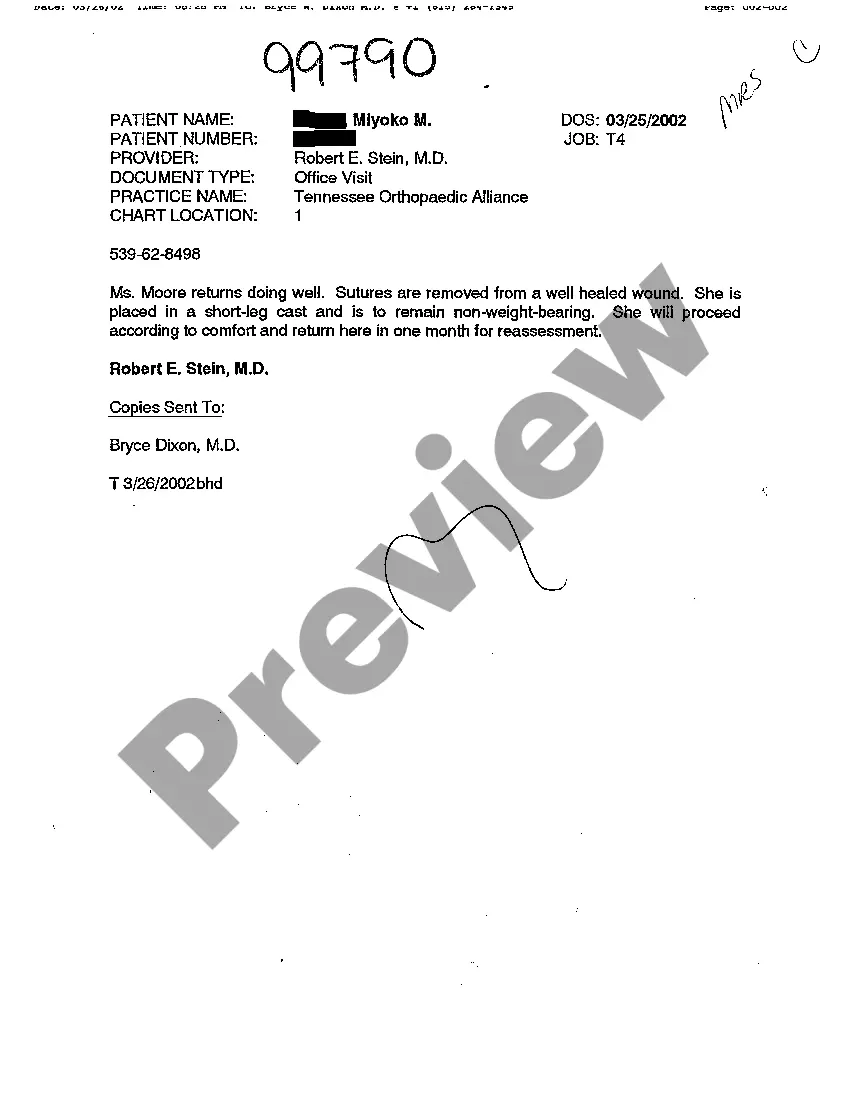
Memphis Tennessee Examination Notes of Treating Physician refer to the detailed records and documentation maintained by a healthcare provider who is responsible for diagnosing and treating patients in Memphis, Tennessee. These examination notes serve as a comprehensive record of a patient's medical history, current health status, and ongoing treatment plan. The Examination Notes of Treating Physician contain relevant information such as the patient's personal details, including their name, age, contact information, and insurance details. It also includes a summary of the patient's chief complaints or reasons for seeking medical attention. Moreover, the notes document the physician's observations during the physical examination, which may include vital signs such as blood pressure, heart rate, respiratory rate, and temperature. They may also include a detailed assessment of the patient's general appearance, cognitive function, and overall well-being. Additionally, the physician's examination notes provide a comprehensive review of the patient's medical history, including past illnesses, surgeries, and significant medical events. It may also encompass information about the patient's family medical history, which can be crucial for identifying potential genetic risk factors. The examination notes of treating physicians in Memphis, Tennessee, are also expected to outline the diagnostic tests conducted or ordered, such as lab tests, imaging studies, or biopsies. The results of these tests are typically recorded in the examination notes, along with the physician's interpretation and analysis. Furthermore, the treating physician documents their medical opinion and proposed treatment plan in these records. This includes prescribing medications, recommending therapies or procedures, and providing guidance on lifestyle modifications or preventive measures. The notes may also include the physician's assessment of the patient's response to previous treatments and any adjustments made to the care plan. Different types of Memphis Tennessee Examination Notes of Treating Physician may include: 1. Initial Visit Examination Notes: These notes are created during a patient's first visit to a new treating physician. They focus on gathering the patient's medical history, conducting a thorough examination, and formulating an initial diagnosis and treatment plan. 2. Progress Examination Notes: These notes are created during subsequent visits or follow-ups with the treating physician. They detail the patient's progress, response to treatment, any changes in symptoms, and adjustments made to the treatment plan. 3. Surgical Examination Notes: These notes are specific to surgical procedures and document the details of the surgery, including preoperative assessments, intraoperative findings, and postoperative care instructions. 4. Specialty-specific Examination Notes: Depending on the specialization of the treating physician, there may be specific examination notes tailored for different medical specialties such as cardiology, neurology, orthopedics, etc. These notes cater to the specific needs and requirements of each medical discipline. In summary, Memphis Tennessee Examination Notes of Treating Physician are comprehensive records that document a patient's medical history, physical examinations, diagnostic tests, treatment plans, and progress. These notes are critical for ensuring continuity of care, facilitating effective communication among healthcare providers, and serving as legal documentation in medical-legal cases.
Memphis Tennessee Examination Notes of Treating Physician
Description
How to fill out Memphis Tennessee Examination Notes Of Treating Physician?
If you are searching for a relevant form, it’s impossible to choose a better platform than the US Legal Forms website – probably the most considerable libraries on the internet. With this library, you can get thousands of form samples for company and personal purposes by categories and regions, or keywords. With our advanced search function, finding the most recent Memphis Tennessee Examination Notes of Treating Physician is as easy as 1-2-3. Additionally, the relevance of each record is verified by a group of professional attorneys that regularly check the templates on our platform and revise them according to the newest state and county laws.
If you already know about our platform and have an account, all you should do to receive the Memphis Tennessee Examination Notes of Treating Physician is to log in to your profile and click the Download button.
If you make use of US Legal Forms for the first time, just follow the instructions below:
- Make sure you have opened the form you want. Read its description and utilize the Preview option (if available) to check its content. If it doesn’t suit your needs, use the Search field at the top of the screen to discover the needed record.
- Confirm your decision. Click the Buy now button. After that, select the preferred subscription plan and provide credentials to register an account.
- Make the purchase. Use your credit card or PayPal account to finish the registration procedure.
- Obtain the form. Pick the file format and download it to your system.
- Make changes. Fill out, revise, print, and sign the received Memphis Tennessee Examination Notes of Treating Physician.
Every form you save in your profile has no expiration date and is yours forever. It is possible to gain access to them using the My Forms menu, so if you need to get an additional duplicate for modifying or creating a hard copy, feel free to come back and export it again at any time.
Make use of the US Legal Forms extensive library to gain access to the Memphis Tennessee Examination Notes of Treating Physician you were seeking and thousands of other professional and state-specific templates on a single platform!