Chattanooga Tennessee Examination Notes of Treating Physician
Description
How to fill out Tennessee Examination Notes Of Treating Physician?
If you have previously accessed our service, sign in to your account and download the Chattanooga Tennessee Examination Notes of Treating Physician onto your device by clicking the Download button. Ensure your subscription is active. If not, renew it according to your payment plan.
If this is your initial encounter with our service, follow these straightforward steps to acquire your document.
You have continuous access to all documents you have purchased: you can find them in your profile under the My documents section whenever you need to retrieve them. Utilize the US Legal Forms service to efficiently find and save any template for your personal or business requirements!
- Ensure you’ve identified the correct document. Review the description and utilize the Preview feature, if offered, to verify if it fulfills your requirements. If it does not, use the Search option above to find the appropriate one.
- Purchase the template. Click the Buy Now button and select a monthly or yearly subscription option.
- Create an account and process the payment. Use your credit card information or the PayPal alternative to finalize the transaction.
- Obtain your Chattanooga Tennessee Examination Notes of Treating Physician. Select the file format for your document and store it on your device.
- Complete your document. Print it out or utilize professional online editors to fill it out and sign it digitally.
Form popularity
FAQ
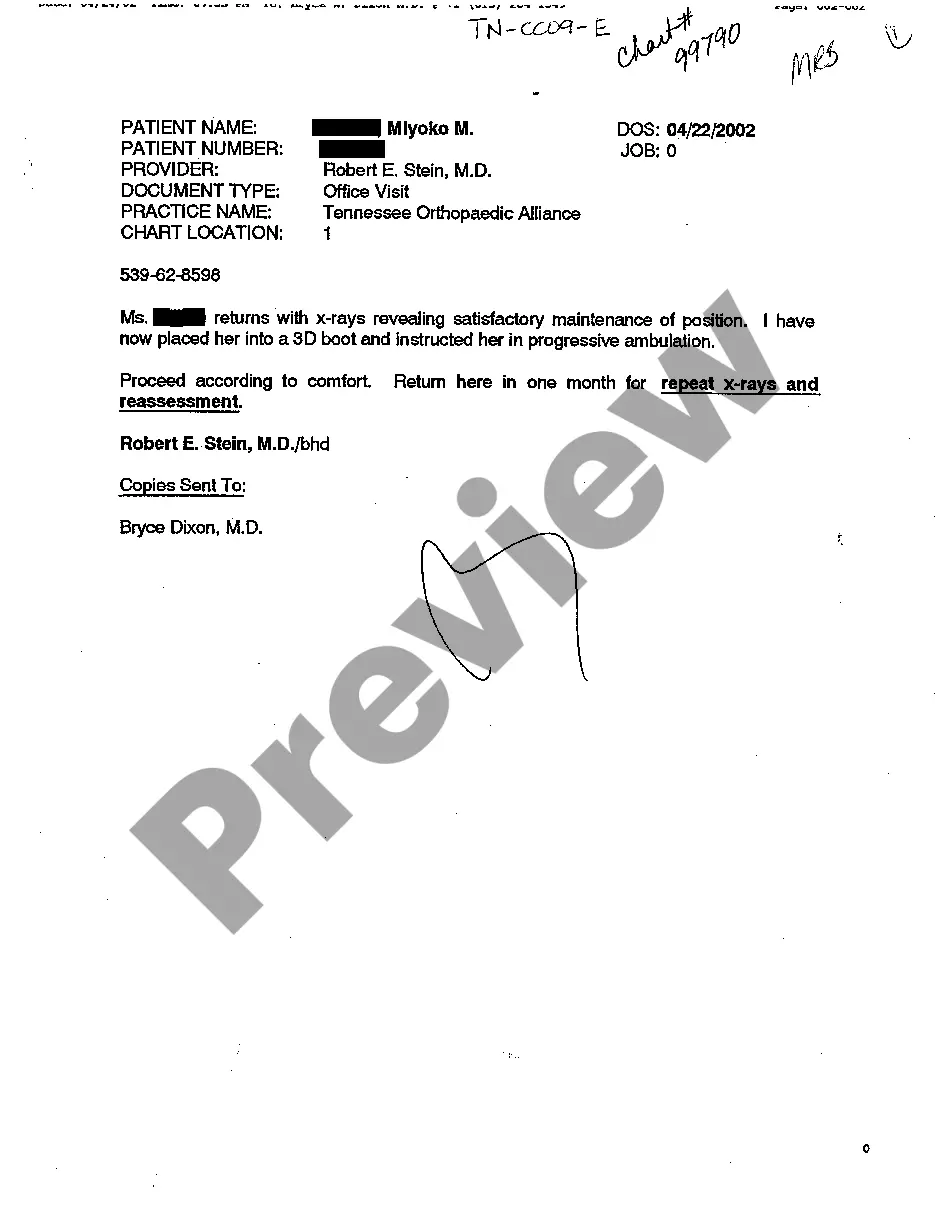
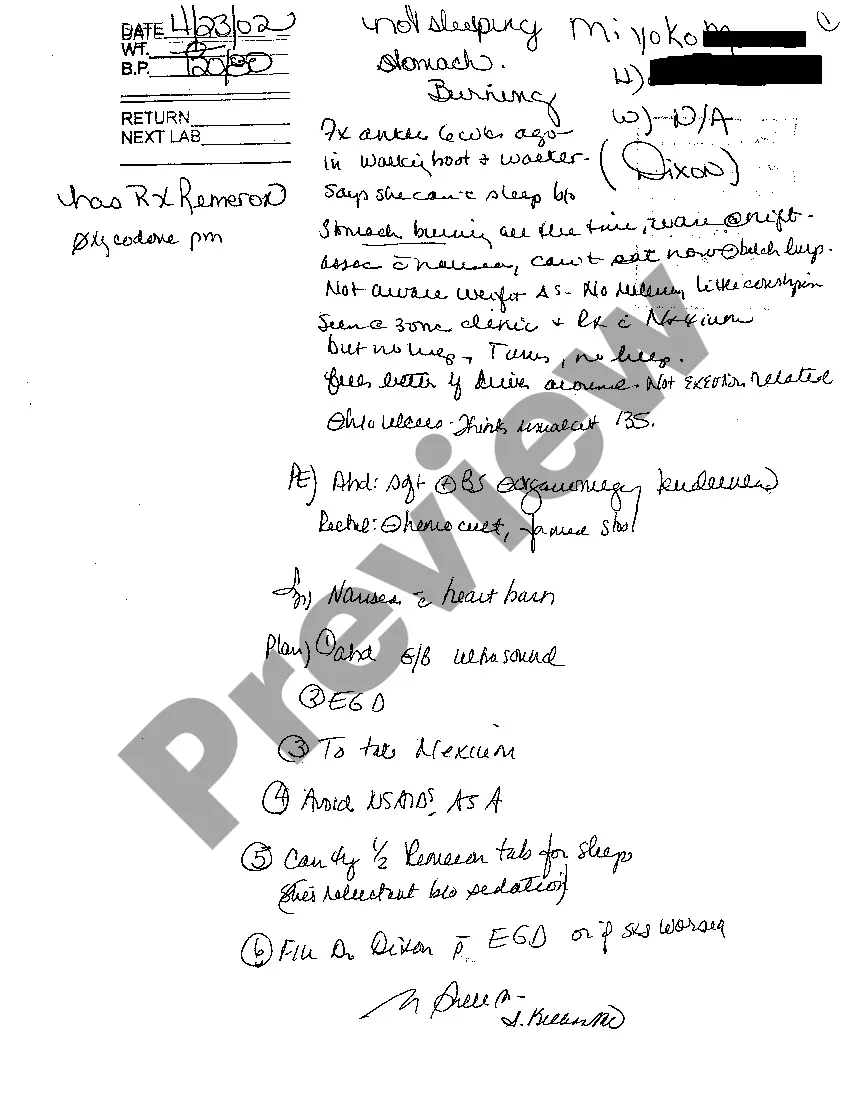
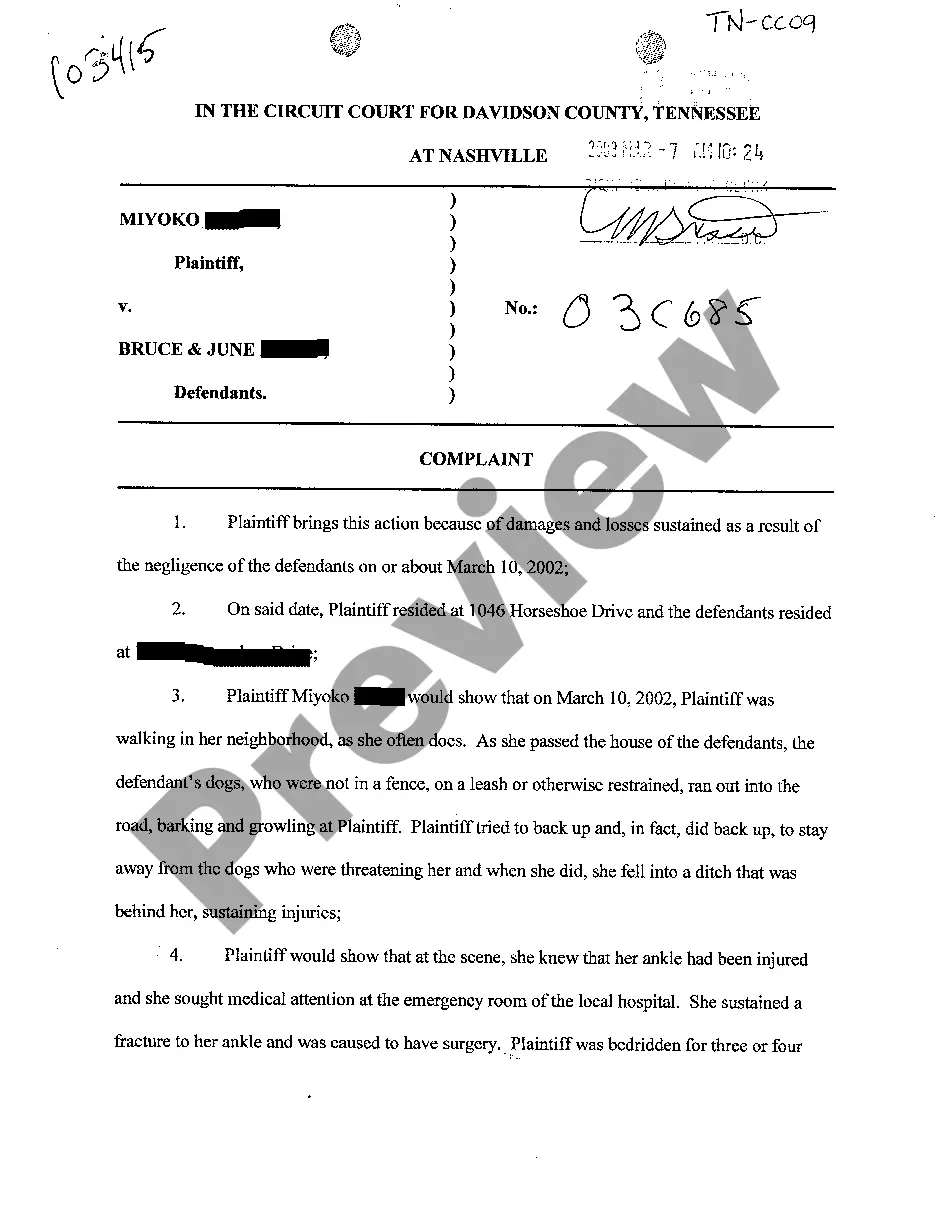
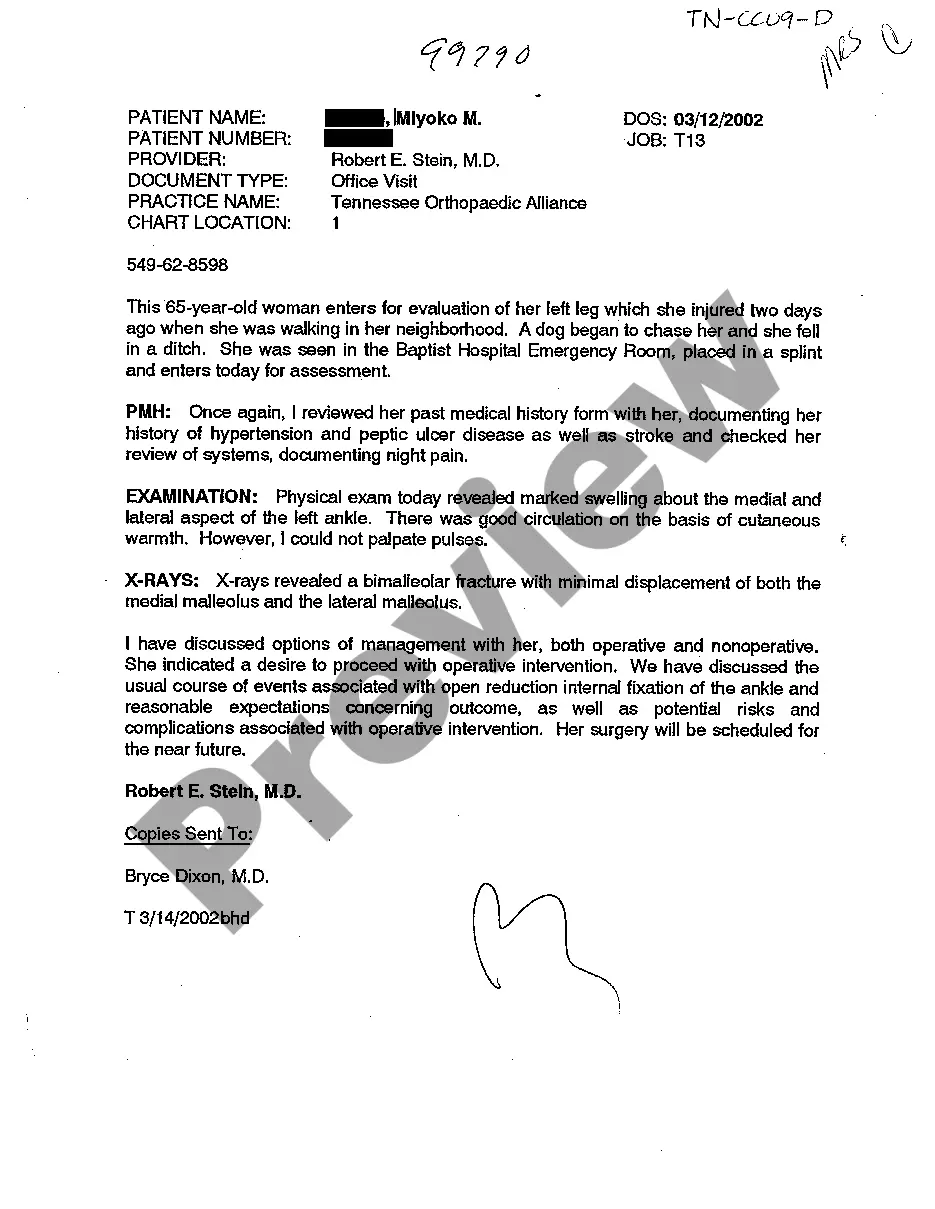
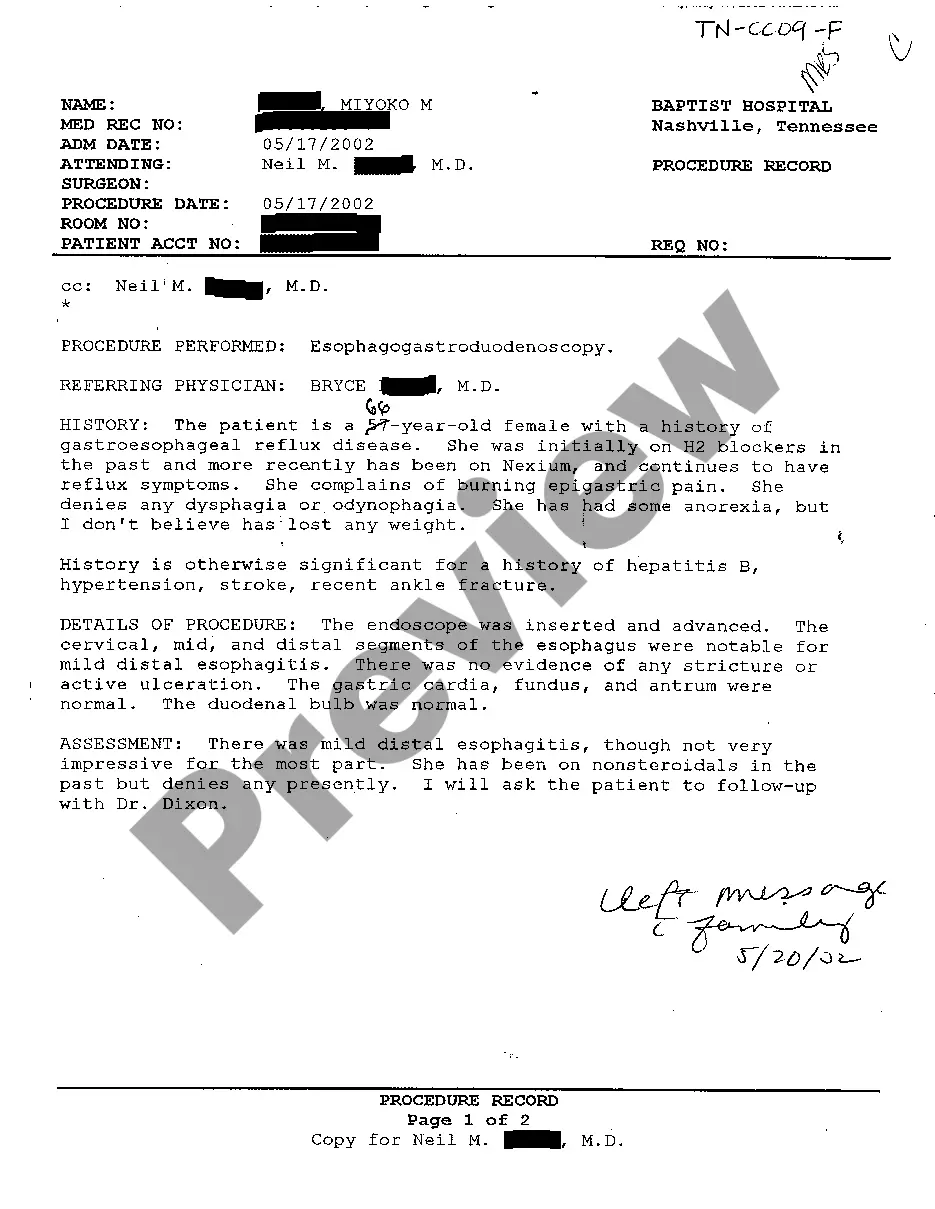
Physician office notes, often referred to as examination notes, are clinical records created during a patient visit. These notes capture vital information regarding the patient's health, examination findings, and treatment plans. They play an important role in ongoing patient care and documentation. Understanding the relevance of Chattanooga Tennessee Examination Notes of Treating Physician can enhance the quality of both care and compliance.
Yes, nurse practitioners can own their own practices in Tennessee, but they must fulfill specific collaboration agreements with a physician. This arrangement ensures that nurse practitioners can operate within the legal frameworks established by the state. It’s beneficial for them to understand how Chattanooga Tennessee Examination Notes of Treating Physician relate to their practice management and documentation.
Ownership laws vary by state; therefore, it’s important to research which states allow non-physicians to own medical practices. Some states have more lenient regulations, permitting ownership under certain circumstances. Generally, states such as Arizona and New Mexico offer more flexibility in this regard. Keep these factors in mind while considering Chattanooga Tennessee Examination Notes of Treating Physician.
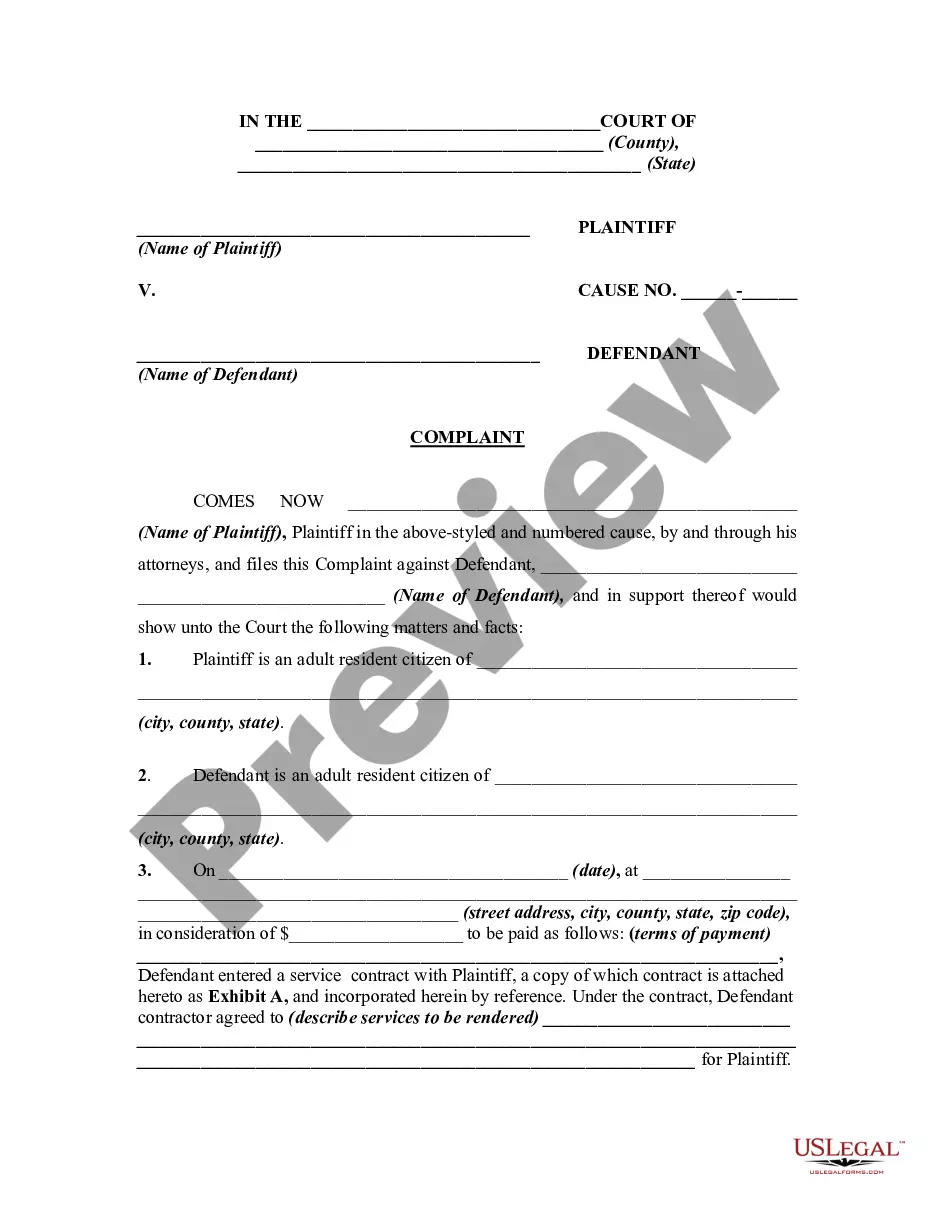
Typically, licensed physicians such as medical doctors (MDs) and doctors of osteopathic medicine (DOs) can own a private practice. They must adhere to state regulations governing medical practice ownership. Additionally, some specialties can have unique arrangements based on the nature of their services. It’s crucial to understand how these regulations may impact your understanding of Chattanooga Tennessee Examination Notes of Treating Physician.
In Tennessee, non-physicians generally cannot own medical practices. The law establishes that healthcare facilities must be owned by licensed physicians. However, there are exceptions for some types of practices, such as those involving limited services. If you're exploring ownership options in the medical field, it's wise to consult with legal experts familiar with Chattanooga Tennessee Examination Notes of Treating Physician for guidance.
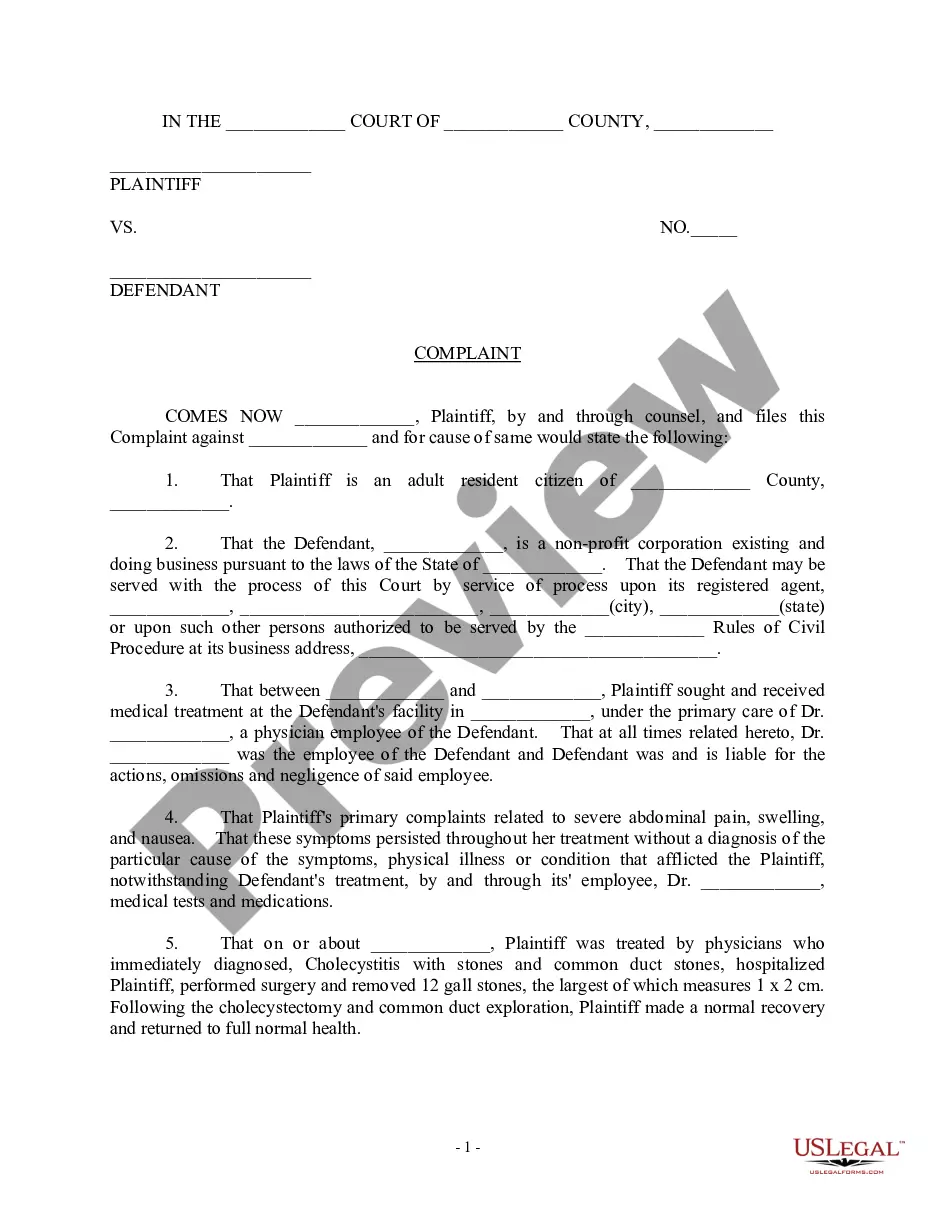
You can report a doctor in Tennessee by contacting the Tennessee Department of Health. It is essential to gather relevant details about the physician, including their name and practice location. Submitting a formal complaint will help initiate the investigation process. These actions may influence Chattanooga Tennessee Examination Notes of Treating Physician concerning the doctor's practices.
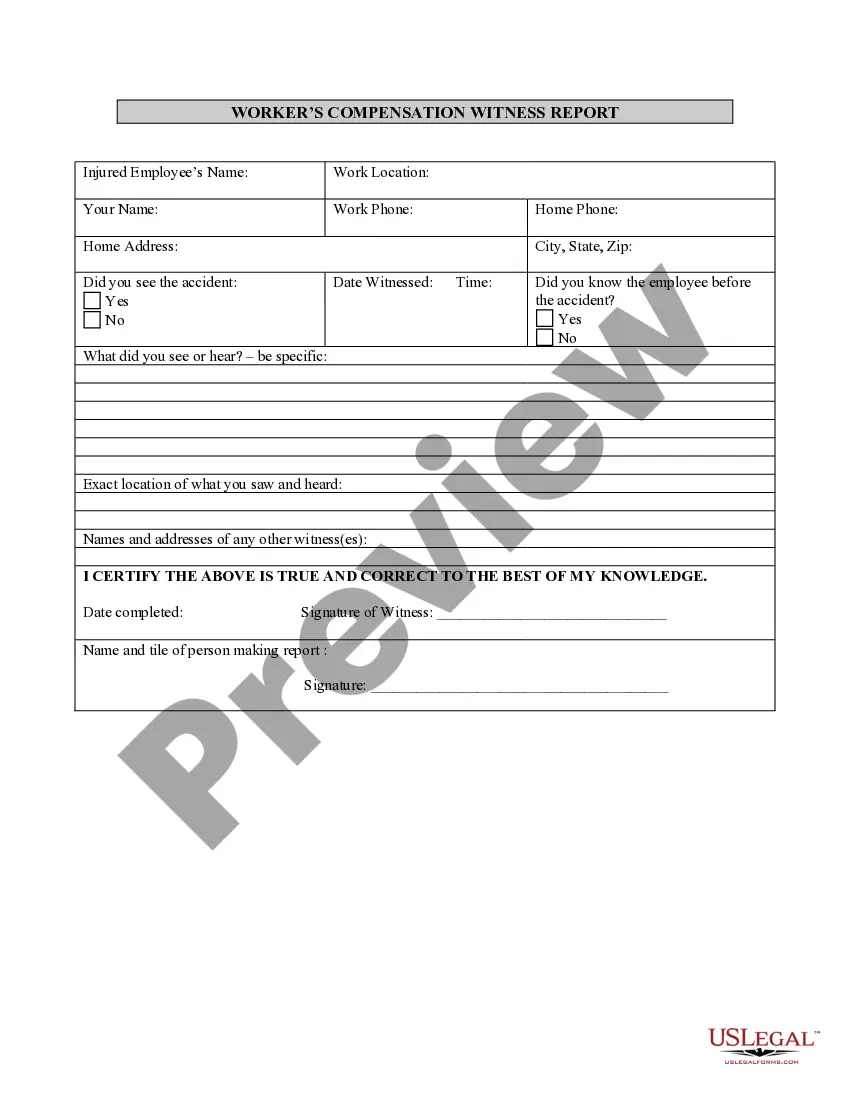
To file an OSHA complaint in Tennessee, visit the OSHA website or contact your local OSHA office. You must provide specific details about the workplace safety issue you are reporting. Protecting workers’ rights is essential, and if applicable, align your complaint with the guidelines found in the Chattanooga Tennessee Examination Notes of Treating Physician for comprehensive insights.
The Tennessee Department of Health oversees public health initiatives, regulates healthcare facilities, and enforces health codes. Their role is crucial in maintaining community health standards. Familiarizing yourself with their functions can guide your understanding of matters related to the Chattanooga Tennessee Examination Notes of Treating Physician.
In Tennessee, non-physicians are generally prohibited from owning a medical practice. However, there are legal avenues available for partnerships and management. If you are considering this route, review the regulations carefully and consider consulting resources like the Chattanooga Tennessee Examination Notes of Treating Physician to ensure compliance.
To report a doctor in Tennessee, you need to file a complaint with the Board of Medical Examiners. You can do this online or by mail, providing detailed information regarding the doctor's conduct or practices. Always keep in mind the importance of relating your findings to the Chattanooga Tennessee Examination Notes of Treating Physician to ensure thoroughness in your report.