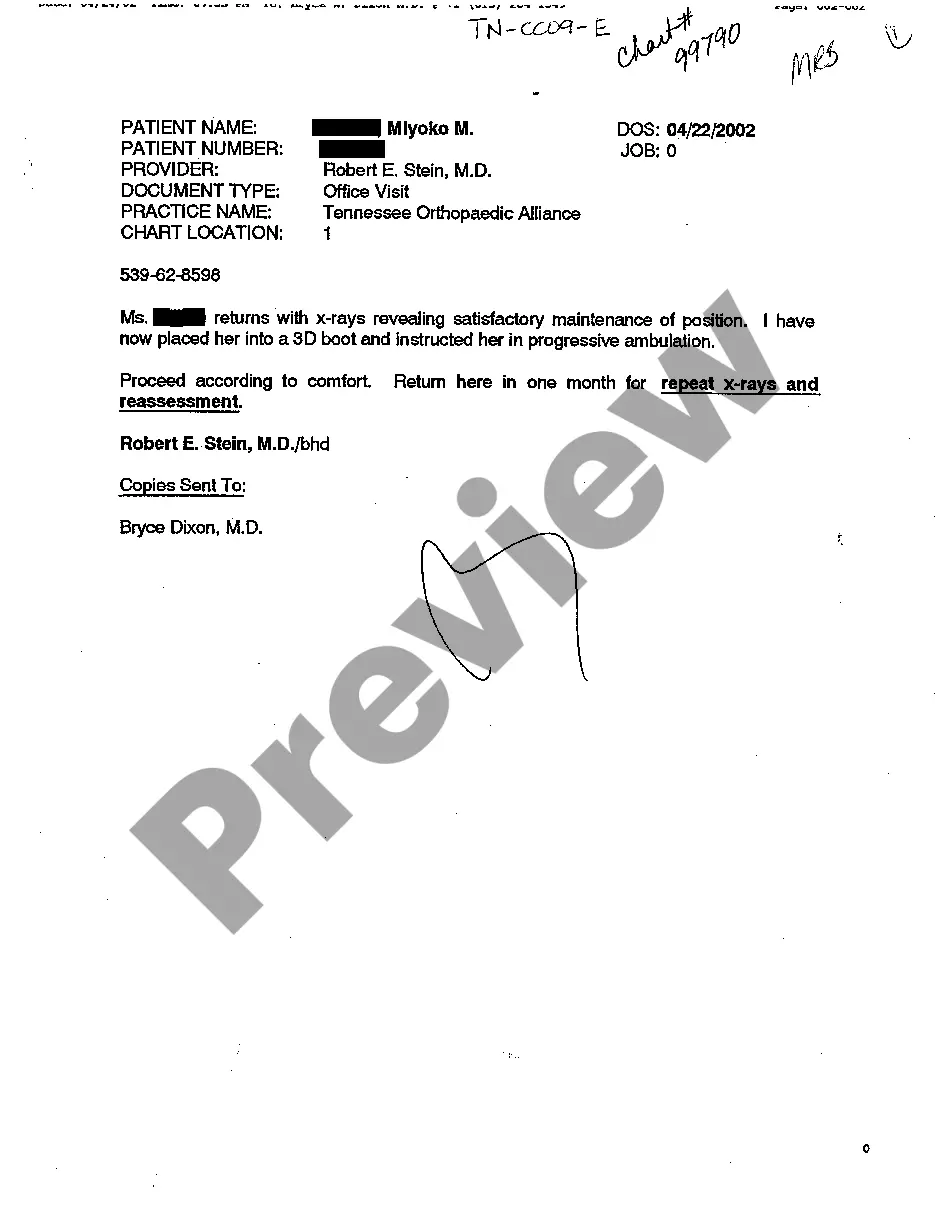
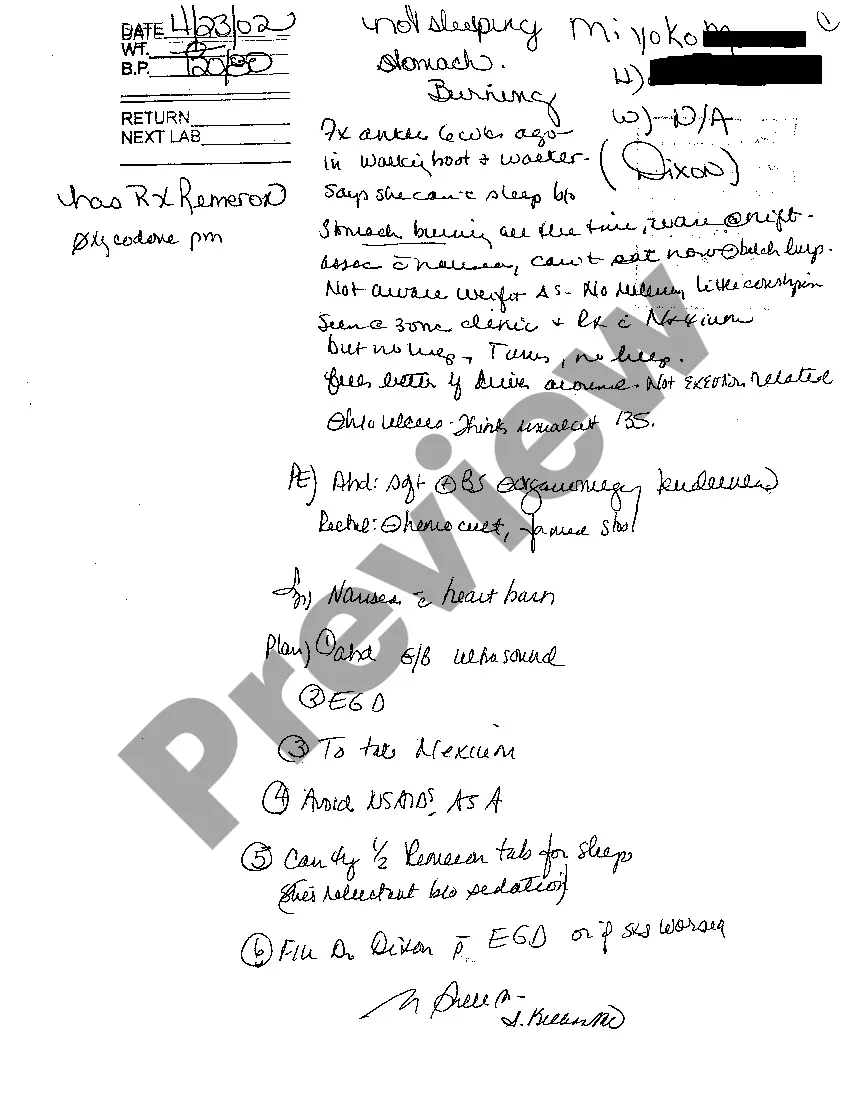
Nashville Tennessee Examination Notes of Treating Physician are detailed records and assessments made by medical professionals in Nashville, Tennessee regarding patients under their care. These examination notes are crucial for monitoring the progress, diagnosis, treatment, and management of patients' medical conditions. The primary purpose of these examination notes is to document all pertinent medical information about the patient's symptoms, medical history, physical examinations, laboratory results, imaging studies, and any procedures or treatments performed. This comprehensive documentation allows the treating physician to have a complete overview of the patient's health status, to make informed clinical decisions, and to monitor the effectiveness of treatment plans. These examination notes typically consist of various types of records, each serving a specific purpose: 1. Initial Examination Notes: These notes are generated during the patient's first visit to the treating physician. They include a detailed account of the patient's medical history, presenting complaints, physical examination findings, and any initial diagnostic tests that may have been conducted to establish a baseline for future comparisons. 2. Progress Examination Notes: These notes are regularly updated by the treating physician to track the patient's progress over time. They document changes in symptoms, response to treatment, adjustments made in the treatment plan, and any additional diagnostic tests conducted. These notes help ensure continuity of care and allow the physician to evaluate the effectiveness of the proposed interventions. 3. Follow-up Examination Notes: These notes are generated during subsequent visits to the treating physician and provide an update on the patient's condition since the last appointment. They include details about any changes in symptoms, side effects of medications, and the overall response to the treatment plan. Follow-up examination notes aid in revising treatment strategies, if necessary, and monitoring the long-term management of the patient's condition. 4. Surgical Examination Notes: In cases where a patient undergoes a surgical procedure, the treating physician will also maintain a separate set of examination notes specifically related to the surgery. These notes provide details regarding the surgical intervention, pre-operative evaluations, post-operative care, and any complications that may have arisen during or after the procedure. In conclusion, Nashville Tennessee Examination Notes of Treating Physician are critical documents that meticulously record a patient's medical information, including diagnoses, treatments, and progress over time. These notes enable physicians to provide comprehensive, informed, and consistent care to their patients, ensuring their health and well-being.
Nashville Tennessee Examination Notes of Treating Physician
Description
How to fill out Nashville Tennessee Examination Notes Of Treating Physician?
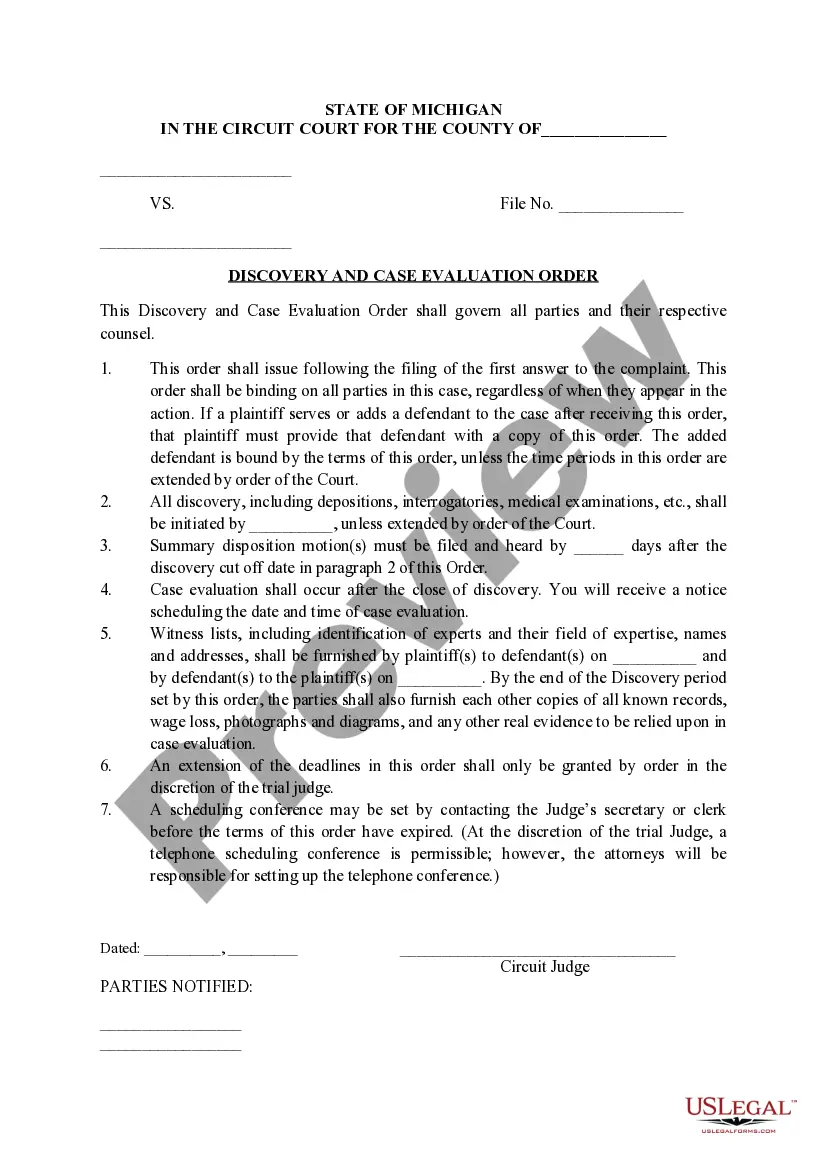
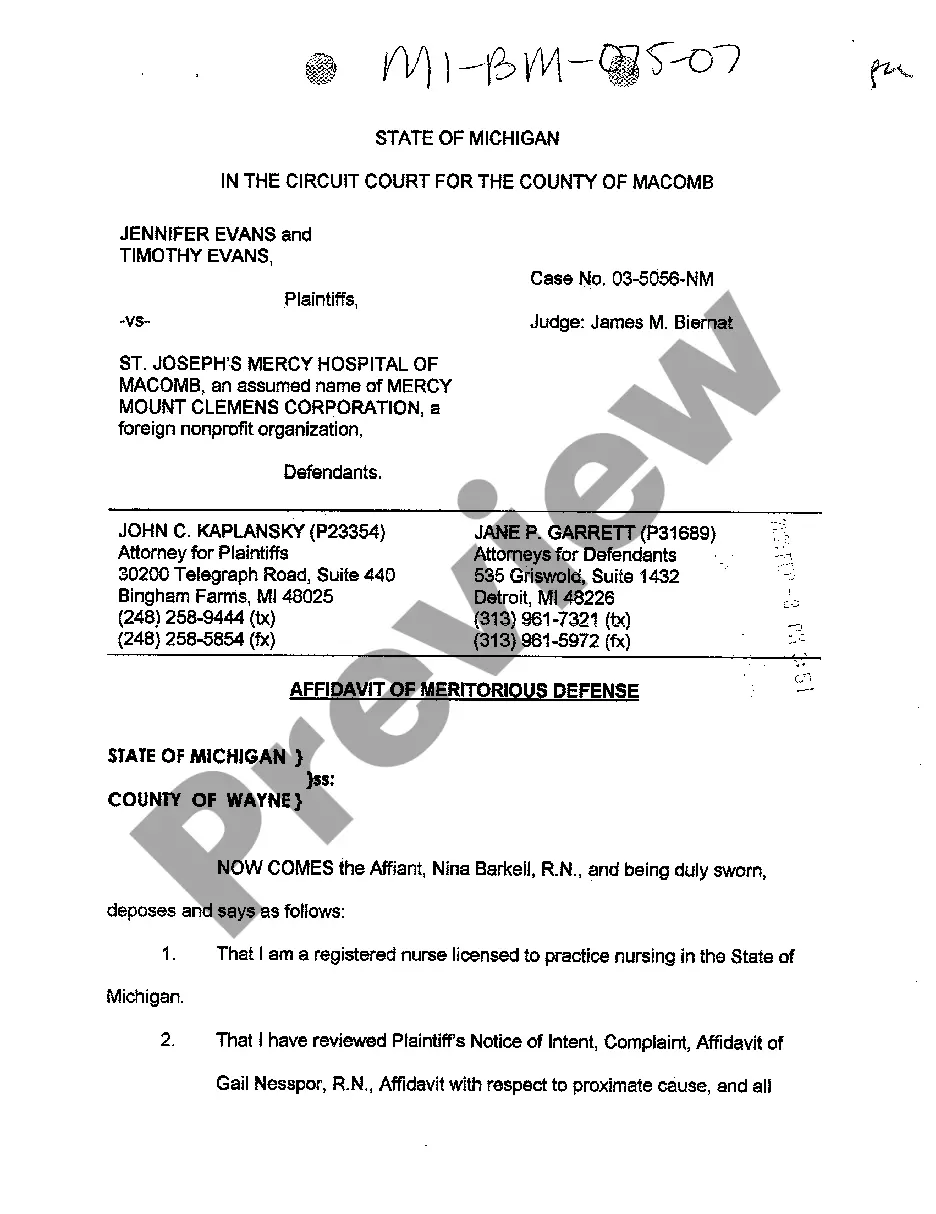
Regardless of an individual’s social or professional rank, filling out legal documents has become an unfortunate requirement in contemporary society. Frequently, it’s nearly impossible for an individual without a legal background to create such documents from scratch, primarily due to the complex terminology and legal subtleties involved. This is where US Legal Forms offers a solution.
Our platform features an extensive collection of over 85,000 state-specific documents ready for use that cater to nearly any legal circumstance. US Legal Forms also proves to be an invaluable resource for associates or legal advisors looking to save time with our DIY documents.
Whether you need the Nashville Tennessee Examination Notes of Treating Physician or any other documents that will be applicable in your region, US Legal Forms makes everything easily accessible. Here’s how you can obtain the Nashville Tennessee Examination Notes of Treating Physician within minutes using our trustworthy service. If you are already a subscriber, feel free to Log In to your account to access the required form.
You’re all set! You can now print the form or complete it online. If you encounter any difficulties finding your purchased documents, you can conveniently access them in the My documents section.
No matter what situation you are attempting to resolve, US Legal Forms has you covered. Give it a try now and experience the benefits for yourself.
- Confirm that the template you have selected is appropriate for your area, as the laws of one state or region may not apply to another.
- Examine the form and review a brief description (if available) of the contexts in which the document can be utilized.
- If the form you picked does not meet your requirements, you can restart the process and search for the needed document.
- Click Buy now and select the subscription option that best fits your needs.
- Log In with your credentials or create a new account from scratch.
- Choose your payment method and proceed to download the Nashville Tennessee Examination Notes of Treating Physician once the payment has been processed.