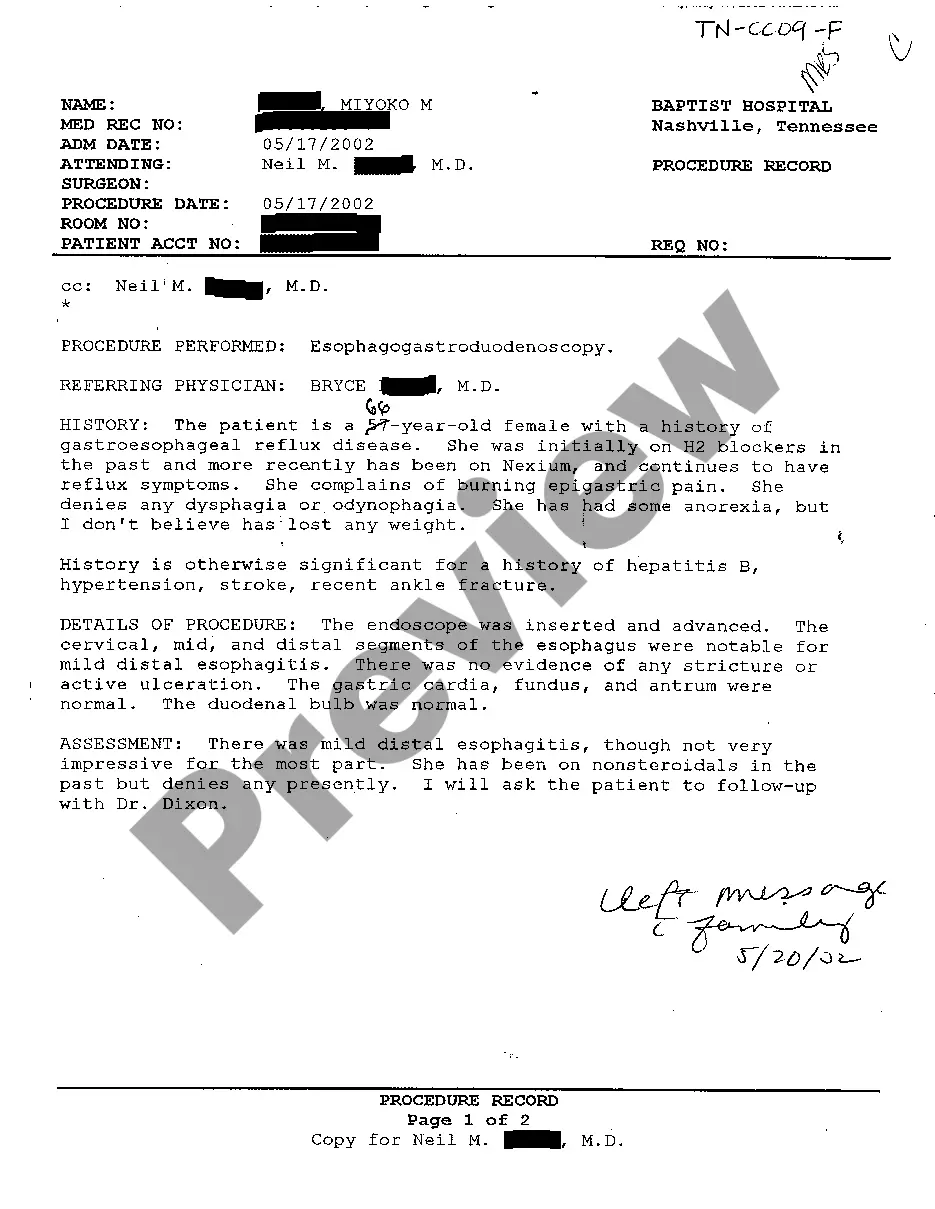
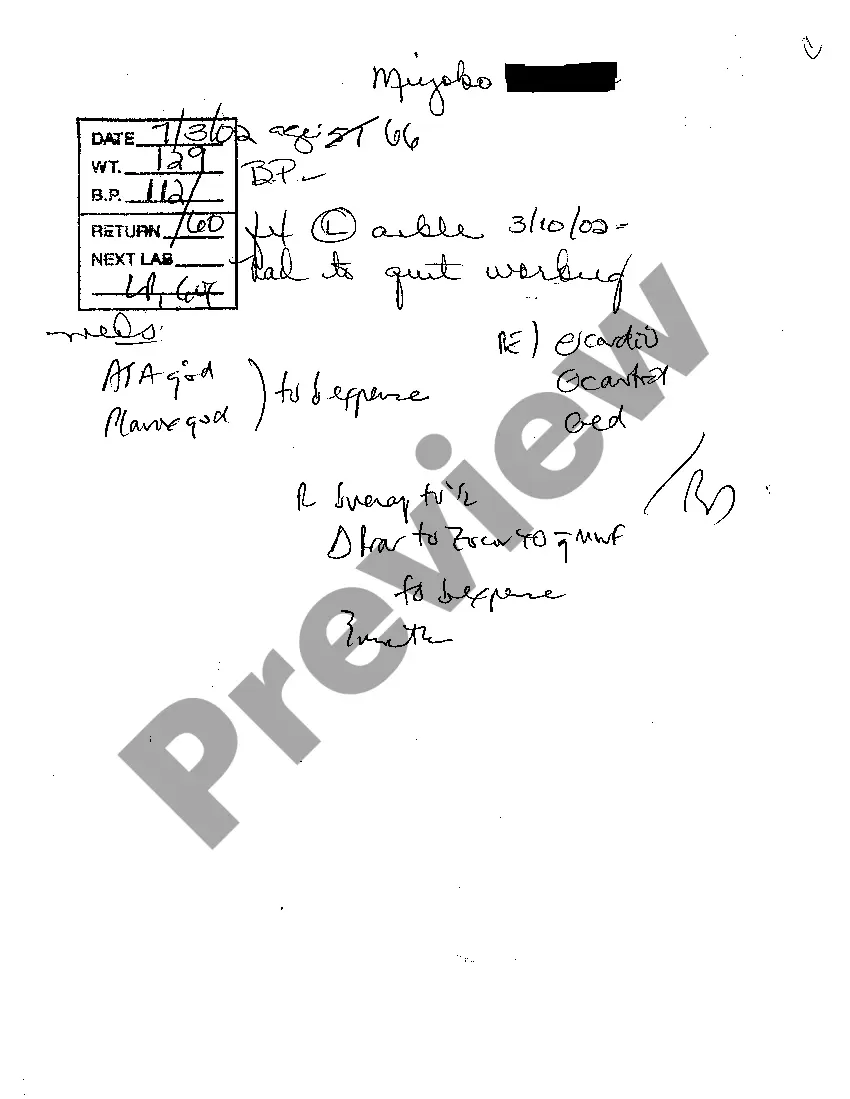
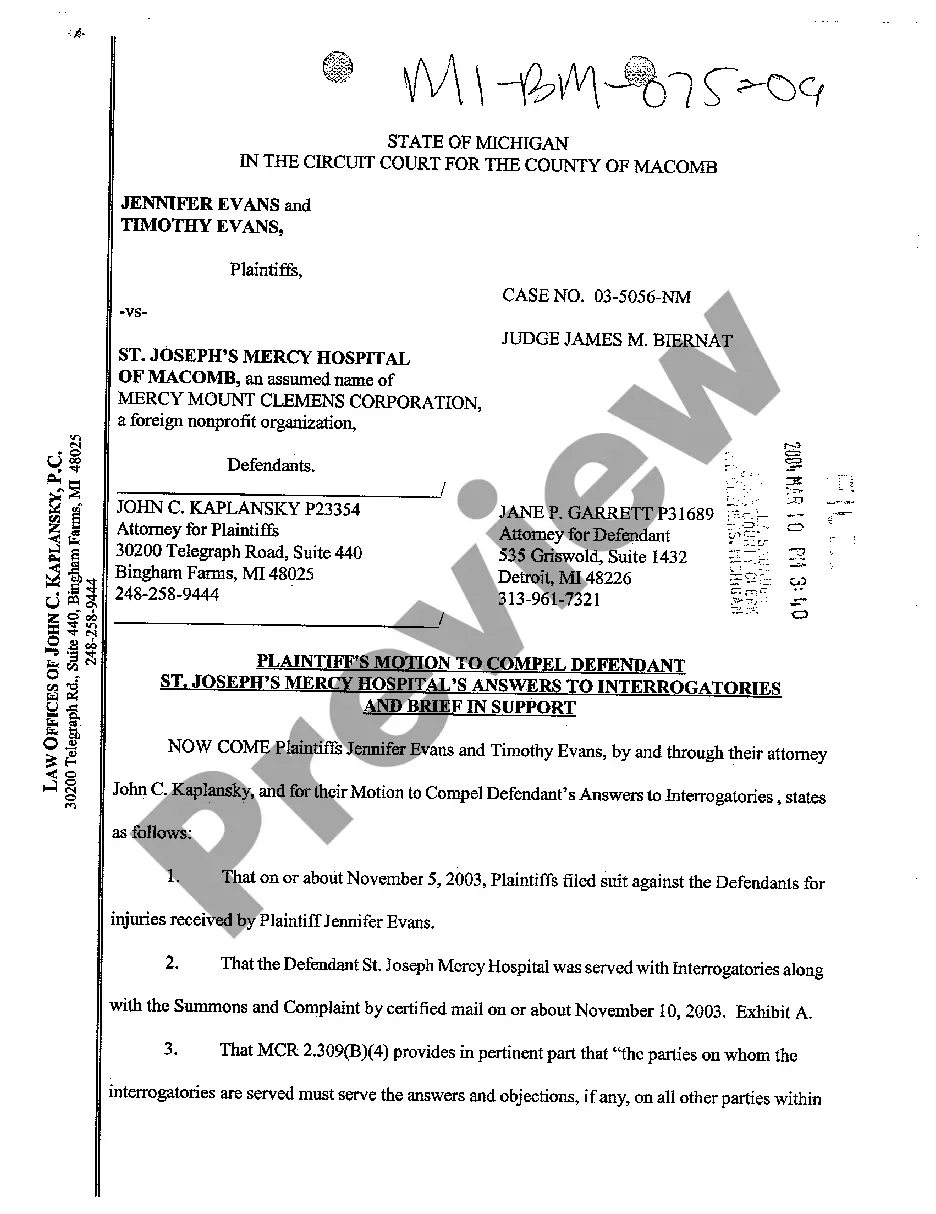
Nashville Tennessee Examination Notes of Treating Physician are comprehensive medical records documenting the evaluations, diagnoses, treatment plans, and progress of patients in Nashville, Tennessee. These examination notes play a crucial role in providing healthcare professionals with valuable insights into a patient's medical history, ongoing conditions, and the effectiveness of their current treatment. The Examination Notes of Treating Physician in Nashville, Tennessee serve to establish a detailed medical narrative, aiding in accurate diagnoses, proper treatment decisions, and effective communication among healthcare providers. These notes are crucial for facilitating continuity of care and ensuring quality healthcare delivery. Types of Nashville Tennessee Examination Notes of Treating Physician include: 1. Initial Examination Notes: These notes are generated during the patient's first visit to the treating physician's office in Nashville, Tennessee. The physician reviews the patient's medical history, performs a physical examination, and records their findings. These notes often include the patient's chief complaints, symptoms, medical history, and initial impressions. 2. Follow-up Examination Notes: These notes are recorded during subsequent visits to the treating physician. They document the progress or changes in the patient's condition, response to previous treatments, and any adjustments made to the treatment plan. Follow-up examination notes help assess the effectiveness of ongoing treatments and ensure appropriate modifications are made if needed. 3. Specialist Consultation Examination Notes: If the treating physician in Nashville, Tennessee refers the patient to a specialist, they receive consultation notes from the specialist, which are incorporated into the patient's examination notes. These notes provide insights into the specialist's opinions, test results, treatment recommendations, or any additional diagnoses made, aiding in a collaborative approach to patient care. 4. Surgical Examination Notes: In cases where surgical intervention is required, these examination notes specifically focus on pre-operative assessments, surgical procedures performed, post-operative care, and progress monitoring. Surgical examination notes provide detailed information regarding the surgery itself, anesthesia considerations, and any complications or adverse effects encountered during the procedure. 5. Mental Health Examination Notes: For patients seeking mental health treatment in Nashville, Tennessee, examination notes from treating physicians specializing in psychiatry or psychology are critical. These notes document psychological evaluations, diagnostic impressions, therapy sessions, prescribed medications, and progress in managing mental health conditions. 6. Rehabilitation Examination Notes: Patients undergoing rehabilitation, such as physical or occupational therapy, have examination notes that monitor their progress, therapeutic modalities utilized, functional improvements, and suggestions for further rehabilitation measures to optimize recovery. 7. Geriatric Examination Notes: Geriatric patients often require specialized care, and these examination notes focus on age-related health issues, chronic condition management, medication assessment, and any necessary modifications to address the unique needs and challenges specific to elderly patients. Overall, Nashville Tennessee Examination Notes of Treating Physician are essential records that enable healthcare providers to make informed decisions concerning patient care. These notes capture valuable medical data throughout the treatment process, fostering effective communication and collaboration in delivering quality healthcare services.
Nashville Tennessee Examination Notes of Treating Physician
Description
How to fill out Nashville Tennessee Examination Notes Of Treating Physician?
Are you looking for a trustworthy and affordable legal forms provider to get the Nashville Tennessee Examination Notes of Treating Physician? US Legal Forms is your go-to solution.
Whether you need a basic agreement to set rules for cohabitating with your partner or a package of documents to move your separation or divorce through the court, we got you covered. Our platform provides over 85,000 up-to-date legal document templates for personal and company use. All templates that we give access to aren’t universal and framed based on the requirements of particular state and county.
To download the form, you need to log in account, locate the required form, and click the Download button next to it. Please keep in mind that you can download your previously purchased document templates at any time from the My Forms tab.
Is the first time you visit our platform? No worries. You can create an account with swift ease, but before that, make sure to do the following:
- Check if the Nashville Tennessee Examination Notes of Treating Physician conforms to the regulations of your state and local area.
- Go through the form’s description (if provided) to find out who and what the form is good for.
- Restart the search if the form isn’t suitable for your legal scenario.
Now you can create your account. Then select the subscription plan and proceed to payment. As soon as the payment is completed, download the Nashville Tennessee Examination Notes of Treating Physician in any provided file format. You can return to the website at any time and redownload the form without any extra costs.
Getting up-to-date legal documents has never been easier. Give US Legal Forms a go today, and forget about wasting hours learning about legal papers online for good.