Cuyahoga Ohio HIPAA Business Associates Agreement is a legally binding contract that outlines the specific responsibilities, obligations, and liabilities of business associates in relation to protected health information (PHI) in accordance with the Health Insurance Portability and Accountability Act (HIPAA). HIPAA, enacted in 1996, aims to safeguard PHI and maintain the privacy and security of individuals' health information. This regulation applies to covered entities such as healthcare providers, health plans, and healthcare clearinghouses. Additionally, any third-party service provider or business associate that handles PHI on behalf of covered entities must comply with HIPAA regulations. Within Cuyahoga County, Ohio, various types of HIPAA Business Associates Agreements may exist to cater to the needs of different entities and organizations. Some common types of agreements include: 1. Healthcare Provider Agreement: This type of agreement is established between a covered healthcare provider and their business associate. It outlines the responsibilities of the business associate in handling and protecting PHI, including restrictions on its use and disclosure, security measures, breach notification requirements, and the business associate's liability in cases of non-compliance. 2. Health Plan Agreement: A health plan or insurance carrier may enter into a HIPAA Business Associates Agreement with their business associate, such as a claims processing company or a utilization review organization. This agreement ensures that the business associate complies with HIPAA regulations while performing services related to the health plan's operations and protects the privacy and security of PHI. 3. IT Service Provider Agreement: Many covered entities rely on IT service providers for various technology-related services, including electronic health record systems, data storage, and network security. In such cases, a HIPAA Business Associates Agreement is essential to define the responsibilities, safeguards, and compliance measures that the IT service provider must adhere to in handling PHI. 4. Medical Billing Agreement: Medical billing companies often handle substantial amounts of PHI on behalf of healthcare providers. A HIPAA Business Associates Agreement between the billing company and the healthcare provider ensures the proper handling, privacy, and security of PHI during the billing process. Regardless of the specific type of Cuyahoga Ohio HIPAA Business Associates Agreement, it must incorporate provisions that address key elements of HIPAA compliance. These include the permitted uses and disclosures of PHI, training and education requirements, safeguards to protect PHI, breach notification protocols, indemnification provisions, and the termination process for non-compliance. It is crucial for all parties involved in a Cuyahoga Ohio HIPAA Business Associates Agreement to thoroughly understand and adhere to their respective roles and responsibilities to protect the integrity and confidentiality of PHI, thereby safeguarding patients' privacy and complying with HIPAA regulations.
Cuyahoga Ohio HIPAA Business Associates Agreement
Description
How to fill out Cuyahoga Ohio HIPAA Business Associates Agreement?
How much time does it usually take you to create a legal document? Given that every state has its laws and regulations for every life scenario, finding a Cuyahoga HIPAA Business Associates Agreement suiting all local requirements can be tiring, and ordering it from a professional lawyer is often expensive. Many web services offer the most popular state-specific documents for download, but using the US Legal Forms library is most advantegeous.
US Legal Forms is the most comprehensive web catalog of templates, grouped by states and areas of use. In addition to the Cuyahoga HIPAA Business Associates Agreement, here you can get any specific document to run your business or personal affairs, complying with your county requirements. Professionals verify all samples for their validity, so you can be sure to prepare your documentation properly.
Using the service is remarkably easy. If you already have an account on the platform and your subscription is valid, you only need to log in, choose the required form, and download it. You can pick the file in your profile at any moment later on. Otherwise, if you are new to the platform, there will be some extra steps to complete before you obtain your Cuyahoga HIPAA Business Associates Agreement:
- Examine the content of the page you’re on.
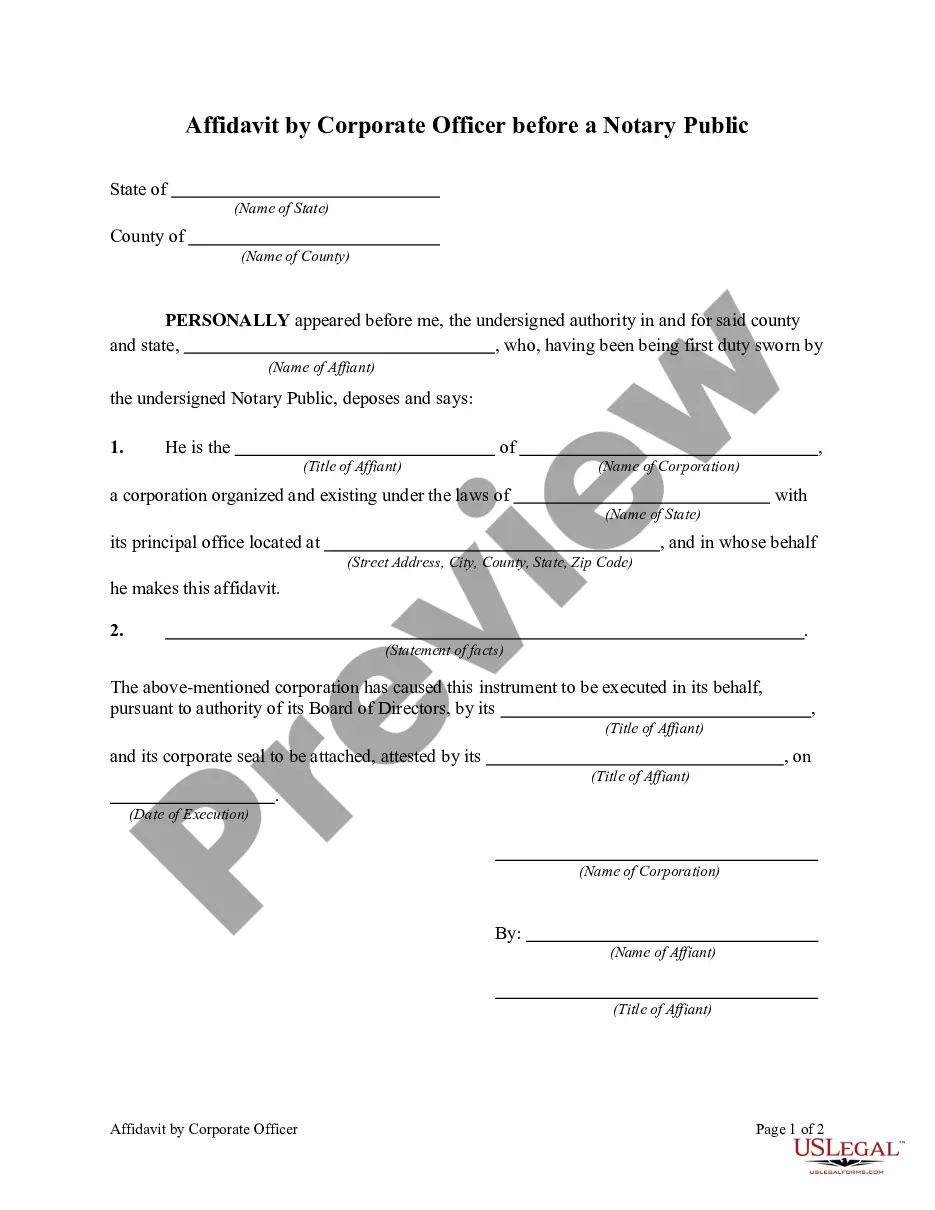
- Read the description of the sample or Preview it (if available).
- Search for another document utilizing the corresponding option in the header.
- Click Buy Now once you’re certain in the selected file.
- Select the subscription plan that suits you most.
- Create an account on the platform or log in to proceed to payment options.
- Pay via PalPal or with your credit card.
- Switch the file format if needed.
- Click Download to save the Cuyahoga HIPAA Business Associates Agreement.
- Print the sample or use any preferred online editor to fill it out electronically.
No matter how many times you need to use the acquired document, you can find all the files you’ve ever saved in your profile by opening the My Forms tab. Give it a try!