This form is a generic example that may be referred to when preparing such a form for your particular state. It is for illustrative purposes only. Local laws should be consulted to determine any specific requirements for such a form in a particular jurisdiction.
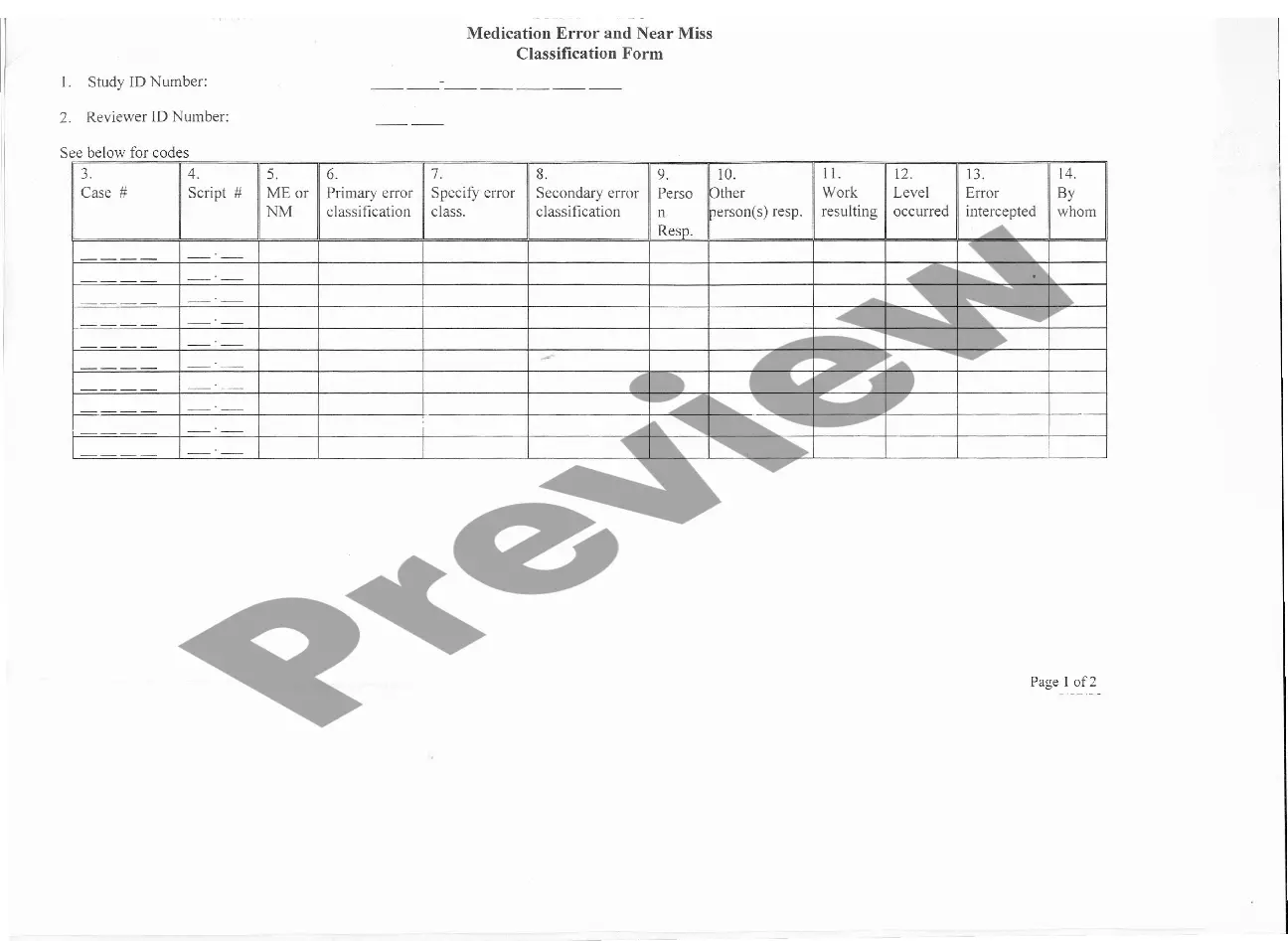
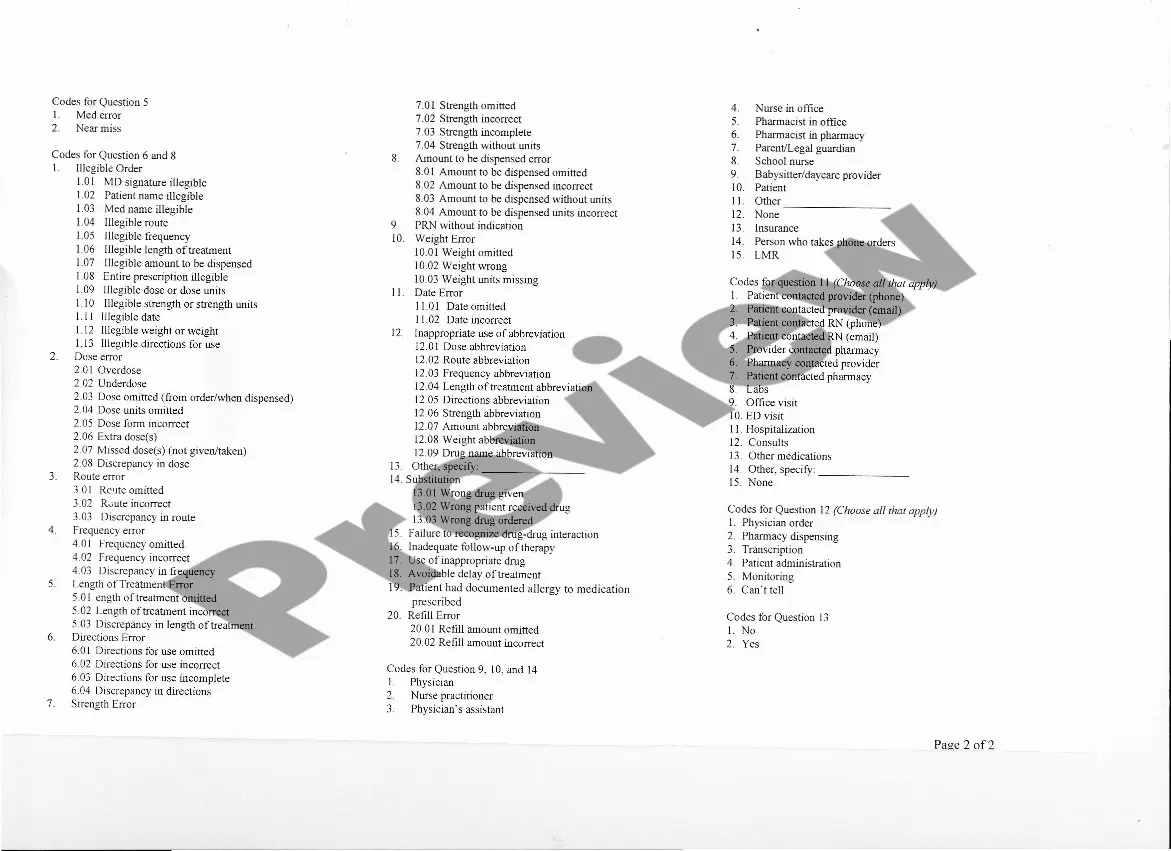
Bronx New York Medication Data Form — Medication Error and Near Miss Classification is a comprehensive document designed to capture relevant information regarding medication errors and near misses that occur in the Bronx, New York area. This form serves as a tool for healthcare professionals to report and analyze incidents in order to improve patient safety and prevent future occurrences. The Medication Error and Near Miss Classification form includes various fields and categories to gather essential data. Relevant keywords for this form may include: 1. Medication Error: This field captures information about incidents involving incorrect medication administration, wrong dosage, or medication administration at the wrong time. It helps identify the scope and impact of errors on patient safety. 2. Near Miss: This category is used to report situations where an error occurred but did not reach the patient, either due to timely intervention or sheer luck. Near misses provide valuable insights into potential vulnerabilities within the medication administration processes. 3. Classification: This section involves classifying the medication error or near miss based on severity, such as minor, moderate, or severe. It helps prioritize incident management and allocate appropriate resources for preventive measures. 4. Medication Type: This field focuses on specifying the type of medication involved in the reported incident, such as antibiotics, analgesics, anticoagulants, or any other relevant drug classes. Analyzing medication-specific errors can facilitate targeted interventions. 5. Contributing Factors: This section helps identify the underlying causes or circumstances that led to the error or near miss. Factors such as communication breakdown, inadequate training, distractions, or system failures are considered. Identifying contributing factors aids in implementing system-wide improvements. 6. Department/Unit: This field captures the department or unit where the incident occurred, enabling data analysis by location. For example, incidents may be categorized by emergency departments, intensive care units, general medicine floors, or outpatient clinics. 7. Time of Incident: This category records the date and time of the medication error or near miss, facilitating temporal analysis. It helps identify peak error-prone periods or identify trends related to specific shifts or times of the day. 8. Outcome: This field records the impact or consequence of the reported incident on the patient. It enables the classification of errors or near misses based on patient harm, such as no harm, temporary harm, or permanent harm. By utilizing the Bronx New York Medication Data Form — Medication Error and Near Miss Classification, healthcare institutions can gather robust data to identify systemic weaknesses, develop targeted interventions, and improve patient safety.