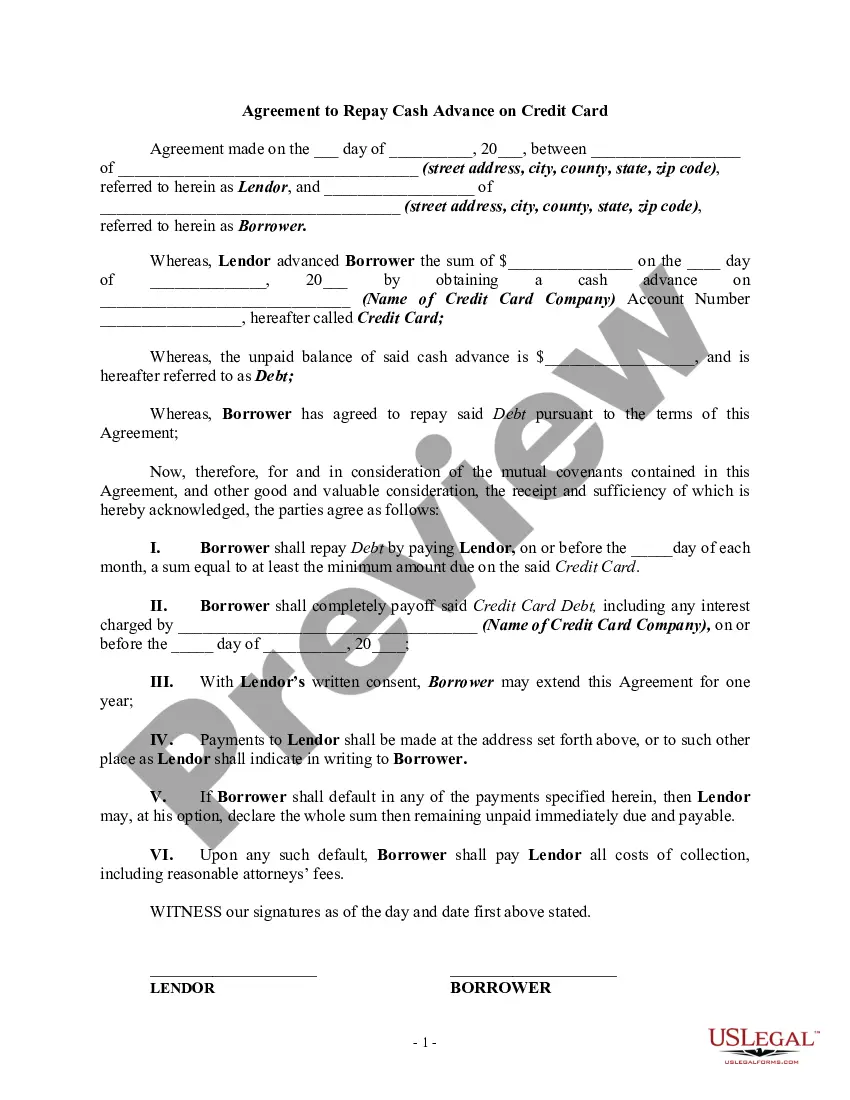
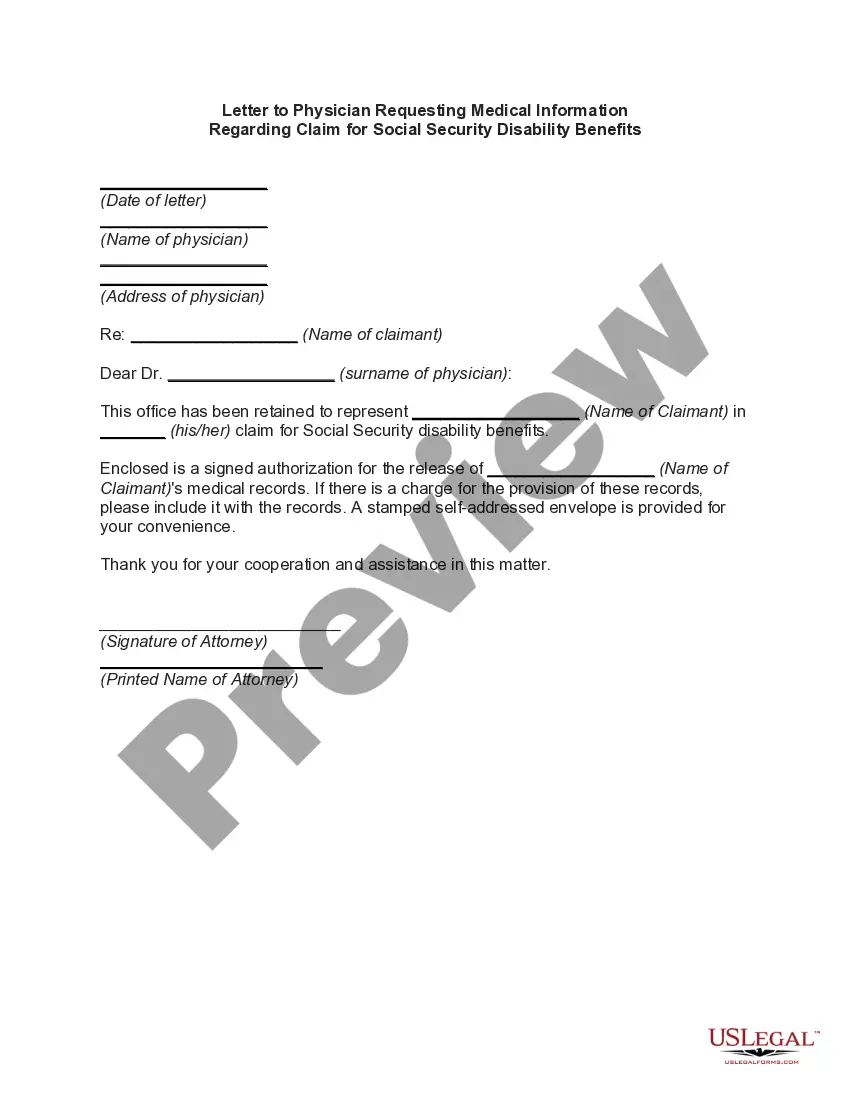
Travis Texas Letter to Physician Requesting Medical Information Regarding Claim for Social Security Disability Benefits is a formal document used in the process of applying for disability benefits from the Social Security Administration (SSA). This letter serves as a request to the claimant's physician for a comprehensive medical report, essential in determining their eligibility for disability benefits. The Travis Texas Letter ensures that all necessary medical information and supporting documentation are obtained to accurately evaluate the claimant's condition, limitations, and ability to work. The letter embodies the crucial role that medical evidence plays in the disability claims process, aiding in the SSA's determination of the claimant's functional capacity to maintain substantial gainful employment. Variations of Travis Texas Letters to Physicians Requesting Medical Information Regarding Claim for Social Security Disability Benefits may include: 1. Initial Request Letter: This type of letter is typically the first correspondence sent to the claimant's physician, urging them to provide a detailed medical report within a specified timeframe. It includes essential information about the claimant's application, such as their name, social security number, and the purpose of the letter. 2. Follow-Up Request Letter: If the initial request letter does not yield a response or if additional information is required, a follow-up letter may be sent. This letter politely reiterates the need for medical documentation while emphasizing the importance of a timely response. It may also offer assistance or address any concerns the physician may have. 3. Specific Medical Records Request Letter: In some cases, the claimant's medical condition may require specific records or test results to support their disability claim. This type of letter would outline the particular documents or information required, such as x-rays, laboratory results, treatment summaries, surgical reports, or psychiatric evaluations. 4. Functional Capacity Assessment Request Letter: To assess a claimant's ability to perform work-related activities given their medical condition, a letter requesting a functional capacity assessment may be necessary. This letter asks the physician to provide an evaluation of the claimant's physical and mental limitations, including the ability to stand, sit, walk, lift, concentrate, and handle job-related stress. It is important to note that variations in wording, formatting, and specific requirements may exist, depending on local regulations and individual circumstances. These letters should always be tailored to meet the specific needs of the claimant and physician involved, ensuring that the necessary medical information is obtained accurately and efficiently.
Travis Texas Letter to Physician Requesting Medical Information Regarding Claim for Social Security Disability Benefits
Description
How to fill out Travis Texas Letter To Physician Requesting Medical Information Regarding Claim For Social Security Disability Benefits?
Whether you plan to open your business, enter into a deal, apply for your ID renewal, or resolve family-related legal issues, you must prepare specific paperwork meeting your local laws and regulations. Locating the correct papers may take a lot of time and effort unless you use the US Legal Forms library.
The service provides users with more than 85,000 expertly drafted and checked legal documents for any individual or business occasion. All files are grouped by state and area of use, so picking a copy like Travis Letter to Physician Requesting Medical Information Regarding Claim for Social Security Disability Benefits is quick and simple.
The US Legal Forms library users only need to log in to their account and click the Download button next to the required template. If you are new to the service, it will take you a couple of more steps to get the Travis Letter to Physician Requesting Medical Information Regarding Claim for Social Security Disability Benefits. Adhere to the guidelines below:
- Make certain the sample meets your individual needs and state law regulations.
- Look through the form description and check the Preview if there’s one on the page.
- Utilize the search tab providing your state above to find another template.
- Click Buy Now to obtain the sample once you find the correct one.
- Opt for the subscription plan that suits you most to proceed.
- Log in to your account and pay the service with a credit card or PayPal.
- Download the Travis Letter to Physician Requesting Medical Information Regarding Claim for Social Security Disability Benefits in the file format you prefer.
- Print the copy or fill it out and sign it electronically via an online editor to save time.
Documents provided by our library are multi-usable. Having an active subscription, you are able to access all of your previously acquired paperwork whenever you need in the My Forms tab of your profile. Stop wasting time on a endless search for up-to-date official documents. Join the US Legal Forms platform and keep your paperwork in order with the most comprehensive online form collection!