Travis Texas Summary of Rights and Obligations under COBRA
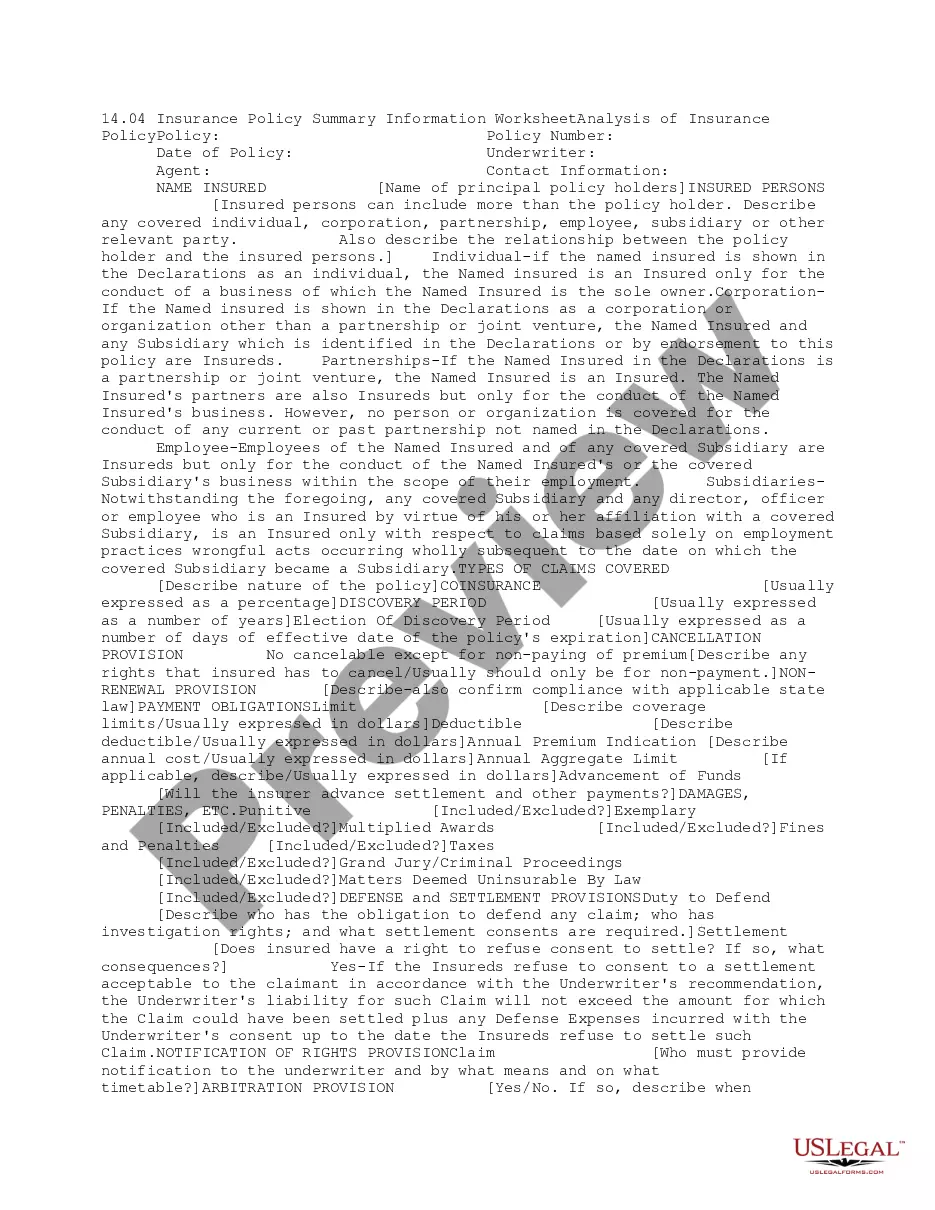
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
Drafting legal documents can be challenging. Additionally, if you choose to hire a lawyer to create a business contract, paperwork for ownership transfer, pre-nuptial agreement, divorce documents, or the Travis Summary of Rights and Responsibilities under COBRA, it might incur significant expenses.
So what is the most sensible approach to conserve time and money while preparing valid documents that fully adhere to your state and local regulations.
Review the form description and utilize the Preview option, if accessible, to verify it's the document you require. If the form does not meet your expectations - search for the appropriate one in the header. Click Buy Now once you identify the needed sample and select the most appropriate subscription. Log In or create an account to purchase your subscription. Complete the payment using a credit card or via PayPal. Choose the file format for your Travis Summary of Rights and Responsibilities under COBRA and save it. Once completed, you can print it out and fill it by hand or upload the templates to an online editor for a quicker and more efficient completion. US Legal Forms allows you to utilize all documents purchased multiple times - you can access your templates in the My documents section of your profile. Give it a try today!
- US Legal Forms is an excellent option, regardless of whether you're looking for forms for personal or commercial purposes.
- US Legal Forms is the largest digital repository of state-specific legal documents, offering users access to the latest verified templates for any application all conveniently in one location.
- Thus, if you require the most current version of the Travis Summary of Rights and Responsibilities under COBRA, you can swiftly find it on our platform.
- Acquiring the documents requires minimal time.
- Existing users should confirm their subscription is active, Log In, and select the template by clicking on the Download button.
- If you're not yet a subscriber, here's how you can obtain the Travis Summary of Rights and Responsibilities under COBRA.
- Browse through the page to check for a template suitable for your region.
Form popularity
FAQ
COBRA continuation coverage may be terminated if we don't receive timely payment of the premium. What is the grace period for monthly COBRA premiums? After election and initial payment, qualified beneficiaries have a 30-day grace period to make monthly payments (that is, 30 days from the due date).
With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
The death of a covered employee is a triggering event for the spouse and covered employee's dependent children to elect COBRA if it causes them to lose coverage. The employer has 30 days after the employee's death to notify the group health plan administrator about the qualifying event.
COBRA allows you to continue coverage typically for up to 18 months after you leave your employer. You can buy an Affordable Care Act (ACA) plan through a public exchange on the health insurance marketplace. Or you can switch to your spouse or partner's plan, if possible.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
If you enroll in COBRA before the 60 days are up, your coverage is then retroactive, as long as you pay the retroactive premiums. This means that if you incur medical bills during your election period, you can retroactively and legally elect COBRA and have those bills covered.
COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too.
Paying for Coverage The cost to the plan is both the portion paid by employees and any portion paid by the employer before the qualifying event. The COBRA premium can equal 100 percent of that combined amount plus a 2 percent administrative fee.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.