The Riverside California COBRA Continuation Coverage Election Form is a crucial document that allows individuals to elect or decline the opportunity to extend their health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). COBRA, a federal law, provides employees and their dependents with the right to continue their employer-sponsored health insurance for a limited period after experiencing a qualifying event that would otherwise result in a loss of coverage. The Riverside California COBRA Continuation Coverage Election Form serves as a formal request from eligible individuals to be enrolled in the COBRA continuation plan. This comprehensive form captures all the essential information required for processing the COBRA coverage, including personal details, employment information, and details about the qualifying event that triggered the need for COBRA. Within the Riverside California COBRA Continuation Coverage Election Form, individuals must specify the type of qualifying event they have experienced, which can include termination of employment, reduction of work hours, divorce or legal separation from the covered employee, or loss of dependent child status. The form might also include options for dependent children who may want to elect coverage independently of the covered employee or spouse. Different versions of the Riverside California COBRA Continuation Coverage Election Form may exist based on specific qualifying events or variations in state regulations. For example, there may be separate forms for individuals who were recently employed and those already on COBRA coverage who have experienced another qualifying event. It is crucial to consult with the specific healthcare plan administrator or employer to obtain the appropriate form for the applicable situation. By completing the Riverside California COBRA Continuation Coverage Election Form accurately and within the designated timeframe, individuals secure their rights to continue receiving healthcare coverage under COBRA. It is essential to carefully review the form's instructions and ensure that all required fields are completed correctly before submitting it to the designated entity, often the employer or health insurance administrator. Failure to submit the form promptly may result in the loss of the option to extend coverage, potentially leaving individuals without health insurance during critical periods of transition.
Riverside California COBRA Continuation Coverage Election Form
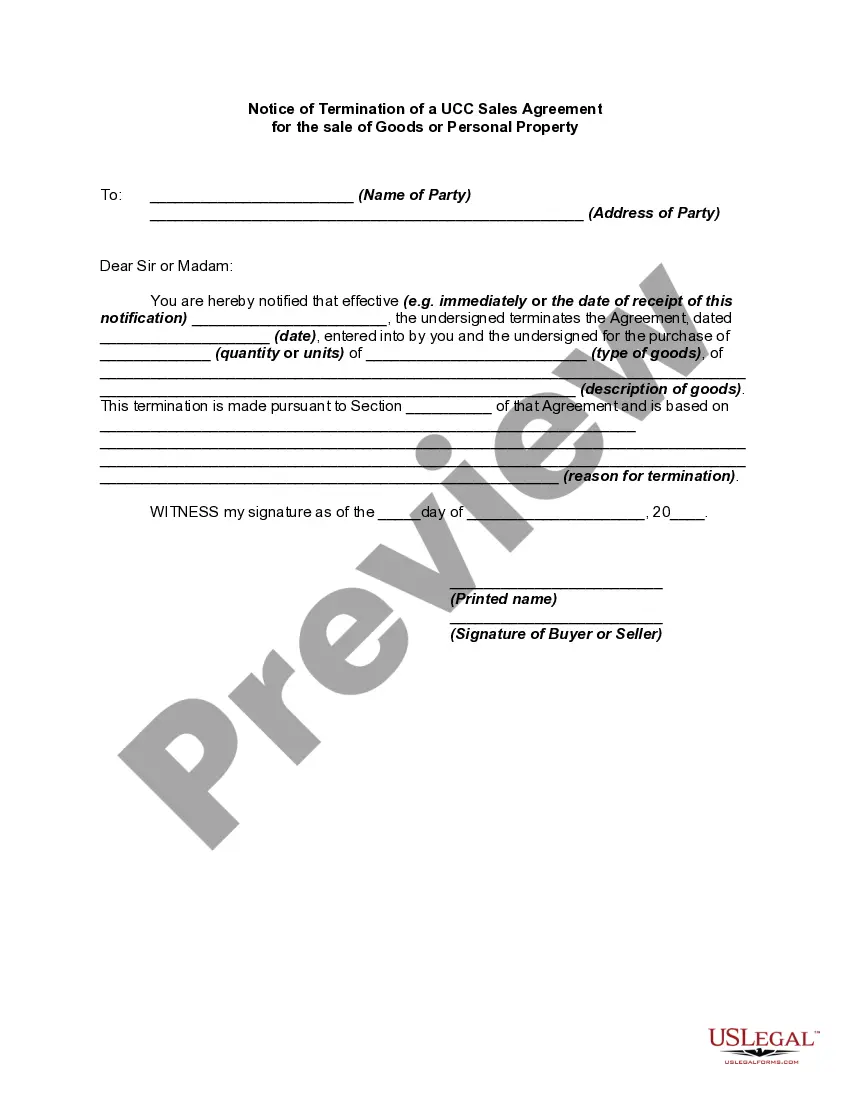
Description
How to fill out Riverside California COBRA Continuation Coverage Election Form?
Preparing documents for the business or personal demands is always a big responsibility. When drawing up an agreement, a public service request, or a power of attorney, it's essential to take into account all federal and state laws of the specific region. However, small counties and even cities also have legislative procedures that you need to consider. All these aspects make it stressful and time-consuming to draft Riverside COBRA Continuation Coverage Election Form without professional help.
It's easy to avoid spending money on lawyers drafting your paperwork and create a legally valid Riverside COBRA Continuation Coverage Election Form on your own, using the US Legal Forms web library. It is the biggest online collection of state-specific legal templates that are professionally verified, so you can be sure of their validity when selecting a sample for your county. Previously subscribed users only need to log in to their accounts to save the needed document.
If you still don't have a subscription, adhere to the step-by-step guideline below to obtain the Riverside COBRA Continuation Coverage Election Form:
- Look through the page you've opened and check if it has the sample you require.
- To do so, use the form description and preview if these options are available.
- To locate the one that fits your needs, use the search tab in the page header.
- Double-check that the sample complies with juridical standards and click Buy Now.
- Opt for the subscription plan, then sign in or register for an account with the US Legal Forms.
- Utilize your credit card or PayPal account to pay for your subscription.
- Download the chosen document in the preferred format, print it, or complete it electronically.
The exceptional thing about the US Legal Forms library is that all the paperwork you've ever purchased never gets lost - you can get it in your profile within the My Forms tab at any moment. Join the platform and quickly obtain verified legal templates for any situation with just a couple of clicks!