Harris Texas COBRA Continuation Coverage Election Notice is a crucial document provided to eligible employees and their dependents in the event of a qualifying event that results in the loss of their employer-sponsored health insurance coverage. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, allows individuals and their families to continue their health benefits for a limited period after certain events occur. The COBRA Continuation Coverage Election Notice specific to Harris Texas serves as a formal communication issued by employers or group health plan administrators. It outlines the rights, options, and necessary steps individuals should take to maintain their health coverage under the COBRA provision. The notice is a vital requirement to ensure affected individuals have access to crucial medical services during times of transition or unexpected job loss. The Harris Texas COBRA Continuation Coverage Election Notice provides clear instructions on the duration of the coverage and the premiums required to maintain it. It is important to note that the notice serves as a notification initiating the COBRA election period, during which individuals can decide whether to opt for COBRA coverage. Different types of Harris Texas COBRA Continuation Coverage Election Notices can be specific to the circumstances triggering eligibility. Some qualifying events that may require issuing this notice include voluntary or involuntary job loss, reduction in work hours, divorce or separation, death of the covered employee, or a dependent child ceasing to meet the plan's eligibility criteria. Harris Texas COBRA Continuation Coverage Election Notices are designed to educate individuals about the continuation of their health insurance coverage under COBRA, emphasizing the need to make a timely decision to avoid disruptions in healthcare services. These notices are tailored to comply with federal regulations and provide the necessary information to make informed decisions about post-employment health benefits. To ensure compliance, employers or group health plan administrators in Harris Texas must carefully review and customize the COBRA Continuation Coverage Election Notice to accurately reflect the terms and conditions of their specific health plans. This helps employees and their eligible dependents understand the available options, costs, and deadlines associated with continuing their health coverage under COBRA. In summary, the Harris Texas COBRA Continuation Coverage Election Notice is a vital document that outlines an individual's rights and responsibilities when faced with certain qualifying events that cause a loss of employer-sponsored health insurance. By providing clear instructions and information, this notice enables individuals to make informed decisions about their healthcare coverage during times of transition, ensuring access to crucial medical services and offering peace of mind.
Harris Texas COBRA Continuation Coverage Election Notice
Description
How to fill out Harris Texas COBRA Continuation Coverage Election Notice?
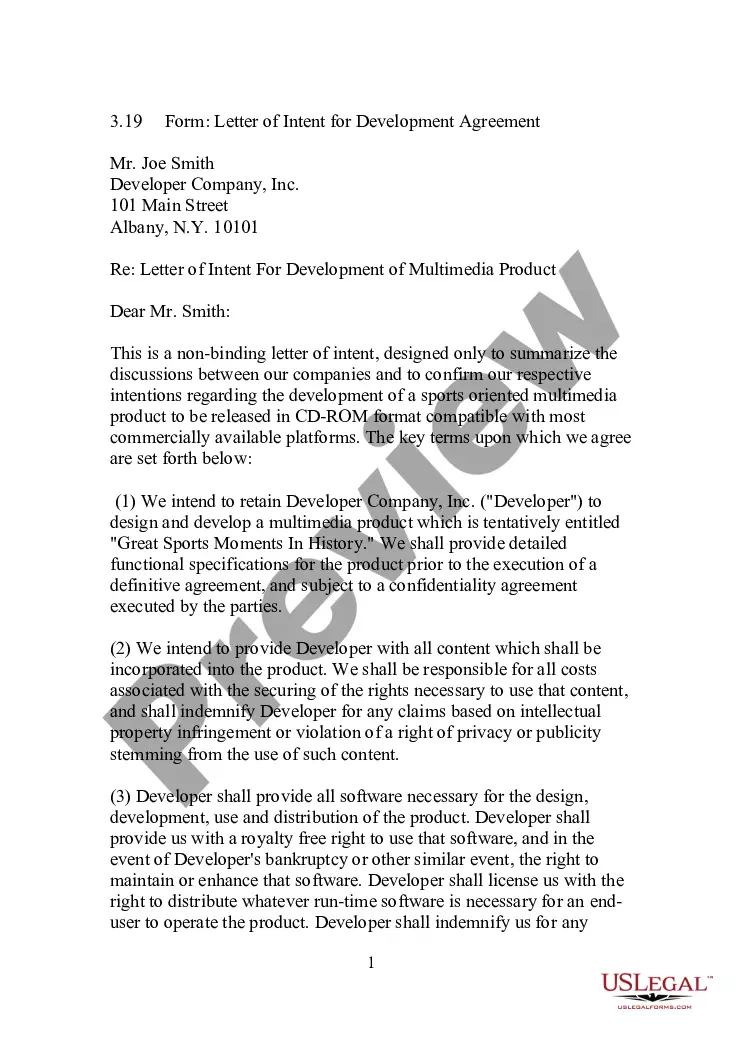
Preparing legal paperwork can be burdensome. Besides, if you decide to ask a legal professional to write a commercial contract, documents for proprietorship transfer, pre-marital agreement, divorce papers, or the Harris COBRA Continuation Coverage Election Notice, it may cost you a lot of money. So what is the best way to save time and money and draft legitimate forms in total compliance with your state and local laws? US Legal Forms is an excellent solution, whether you're looking for templates for your personal or business needs.
US Legal Forms is the most extensive online library of state-specific legal documents, providing users with the up-to-date and professionally checked forms for any use case collected all in one place. Consequently, if you need the current version of the Harris COBRA Continuation Coverage Election Notice, you can easily locate it on our platform. Obtaining the papers takes a minimum of time. Those who already have an account should check their subscription to be valid, log in, and pick the sample with the Download button. If you haven't subscribed yet, here's how you can get the Harris COBRA Continuation Coverage Election Notice:
- Look through the page and verify there is a sample for your region.
- Examine the form description and use the Preview option, if available, to make sure it's the template you need.
- Don't worry if the form doesn't suit your requirements - look for the correct one in the header.
- Click Buy Now when you find the required sample and choose the best suitable subscription.
- Log in or register for an account to pay for your subscription.
- Make a transaction with a credit card or through PayPal.
- Choose the file format for your Harris COBRA Continuation Coverage Election Notice and save it.
When finished, you can print it out and complete it on paper or upload the samples to an online editor for a faster and more practical fill-out. US Legal Forms enables you to use all the documents ever purchased many times - you can find your templates in the My Forms tab in your profile. Try it out now!