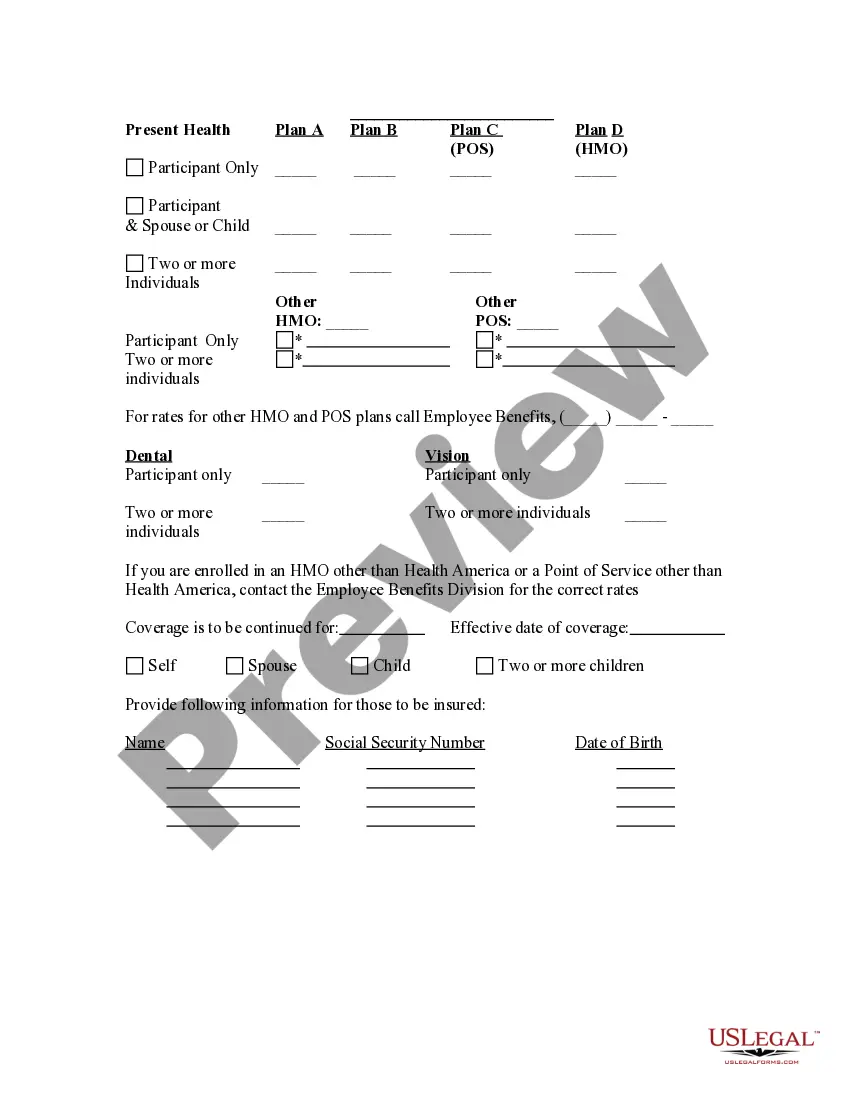
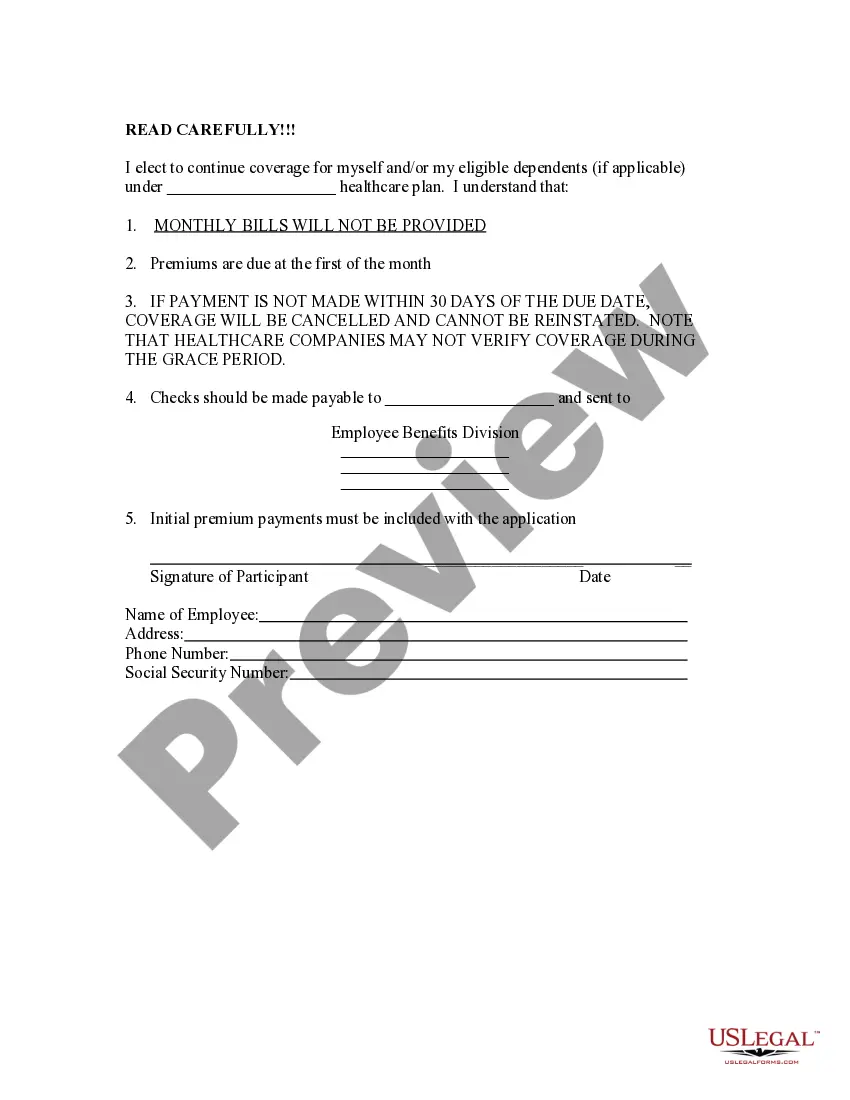
The Alameda California Election Form for Continuation of Benefits — COBRA is a crucial document that enables eligible individuals to select and continue their health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA) in Alameda, California. COBRA provides employees, retirees, and their dependents who lose their group health coverage due to qualifying events such as job loss, reduction in work hours, or other specified circumstances with the option to retain their health insurance for a limited period. It ensures that these individuals can continue to receive important medical services and maintain their health coverage during periods of transition. The Alameda California Election Form for Continuation of Benefits — COBRA outlines the necessary information that individuals need to provide when electing to continue their health insurance under COBRA. This form typically requires personal details such as the employee's name, address, social security number, and the date when coverage originally commenced. Moreover, this form may include a section to indicate the type of qualifying event triggering the need for COBRA coverage continuation. For instance, individuals may need to specify if their job termination, divorce, or reduction in work hours led to the loss of their health insurance. This detail helps the employer or health plan administrator to accurately determine the eligibility for COBRA continuation. Additionally, the Alameda California Election Form for Continuation of Benefits — COBRA may include information regarding the available COBRA coverage options. This can involve selecting the specific health plan option, such as individual or family coverage, and at times, the opportunity to modify the plan based on personal needs. It is essential to note that there may not be different types of Alameda California Election Forms for Continuation of Benefits — COBRA. However, the content and structure of the form may vary slightly depending on the employer or health plan administrator. In some cases, the form may be customized to include additional fields or instructions specific to a particular organization. In conclusion, the Alameda California Election Form for Continuation of Benefits — COBRA is a fundamental document that allows individuals in Alameda, California, to continue their health insurance coverage under COBRA. By completing this form accurately, eligible individuals can ensure the uninterrupted access to necessary healthcare services during critical times of transition.
Alameda California Election Form for Continuation of Benefits - COBRA
Description
How to fill out Alameda California Election Form For Continuation Of Benefits - COBRA?
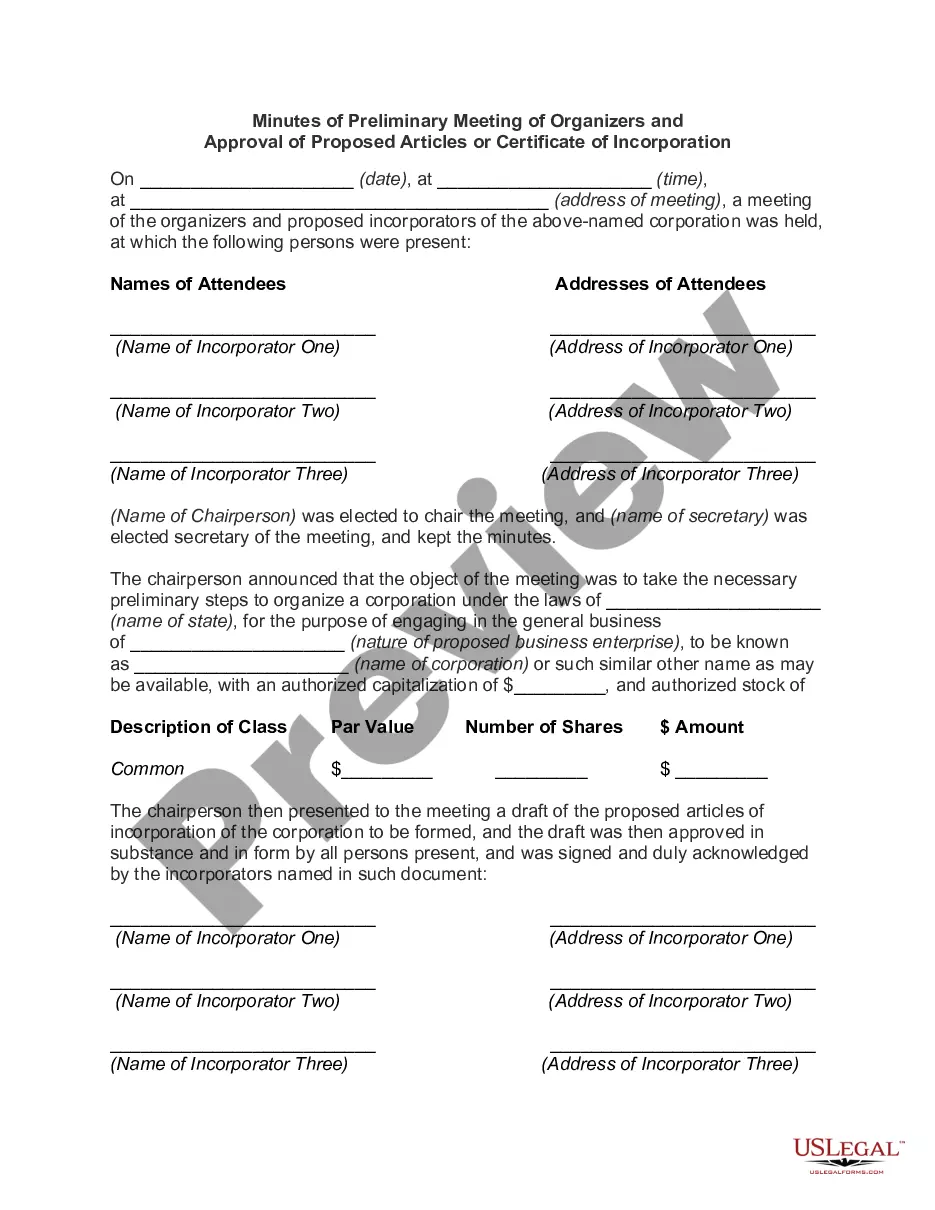
Creating paperwork, like Alameda Election Form for Continuation of Benefits - COBRA, to take care of your legal matters is a challenging and time-consumming task. A lot of circumstances require an attorney’s participation, which also makes this task not really affordable. Nevertheless, you can take your legal issues into your own hands and take care of them yourself. US Legal Forms is here to save the day. Our website comes with more than 85,000 legal documents crafted for a variety of scenarios and life situations. We make sure each document is compliant with the regulations of each state, so you don’t have to worry about potential legal problems associated with compliance.
If you're already familiar with our services and have a subscription with US, you know how straightforward it is to get the Alameda Election Form for Continuation of Benefits - COBRA template. Simply log in to your account, download the template, and personalize it to your needs. Have you lost your document? Don’t worry. You can find it in the My Forms folder in your account - on desktop or mobile.
The onboarding process of new customers is fairly simple! Here’s what you need to do before getting Alameda Election Form for Continuation of Benefits - COBRA:
- Make sure that your form is specific to your state/county since the regulations for writing legal documents may differ from one state another.
- Discover more information about the form by previewing it or reading a quick description. If the Alameda Election Form for Continuation of Benefits - COBRA isn’t something you were hoping to find, then use the header to find another one.
- Log in or create an account to begin using our service and get the form.
- Everything looks great on your side? Click the Buy now button and choose the subscription option.
- Select the payment gateway and type in your payment information.
- Your form is all set. You can go ahead and download it.
It’s an easy task to find and buy the appropriate document with US Legal Forms. Thousands of businesses and individuals are already benefiting from our extensive collection. Sign up for it now if you want to check what other perks you can get with US Legal Forms!