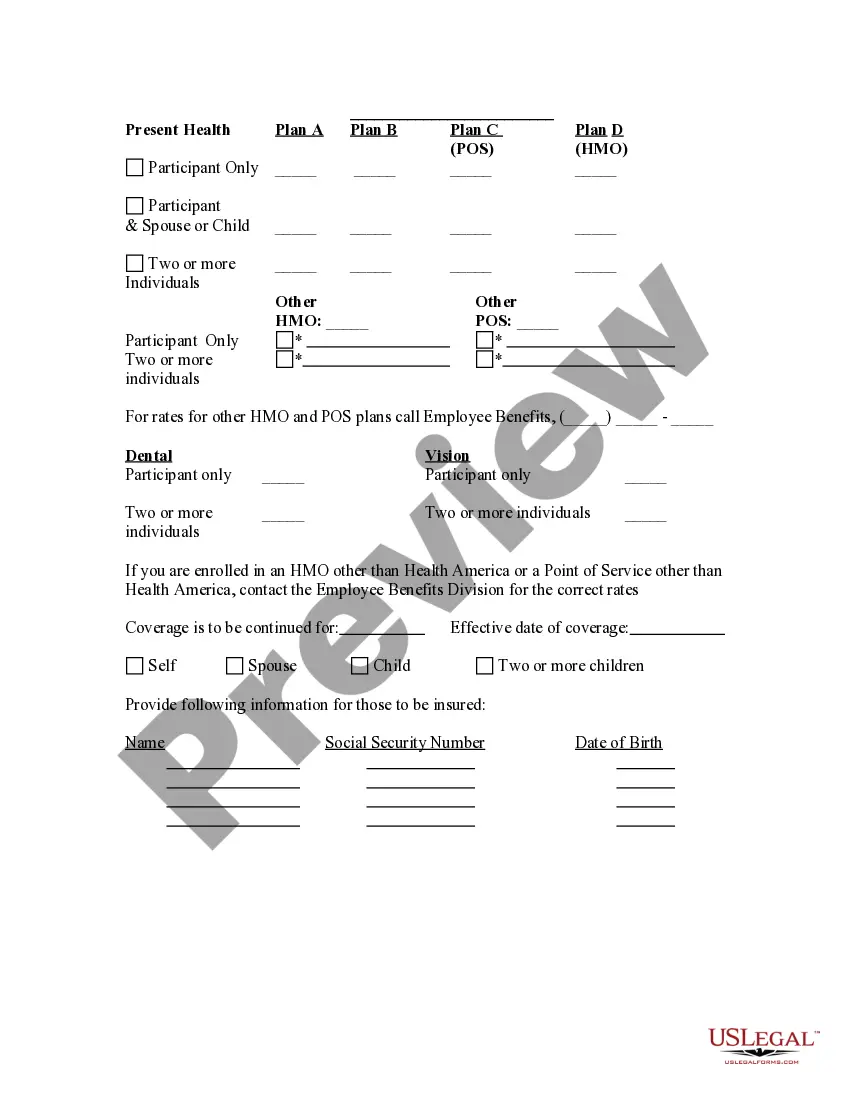
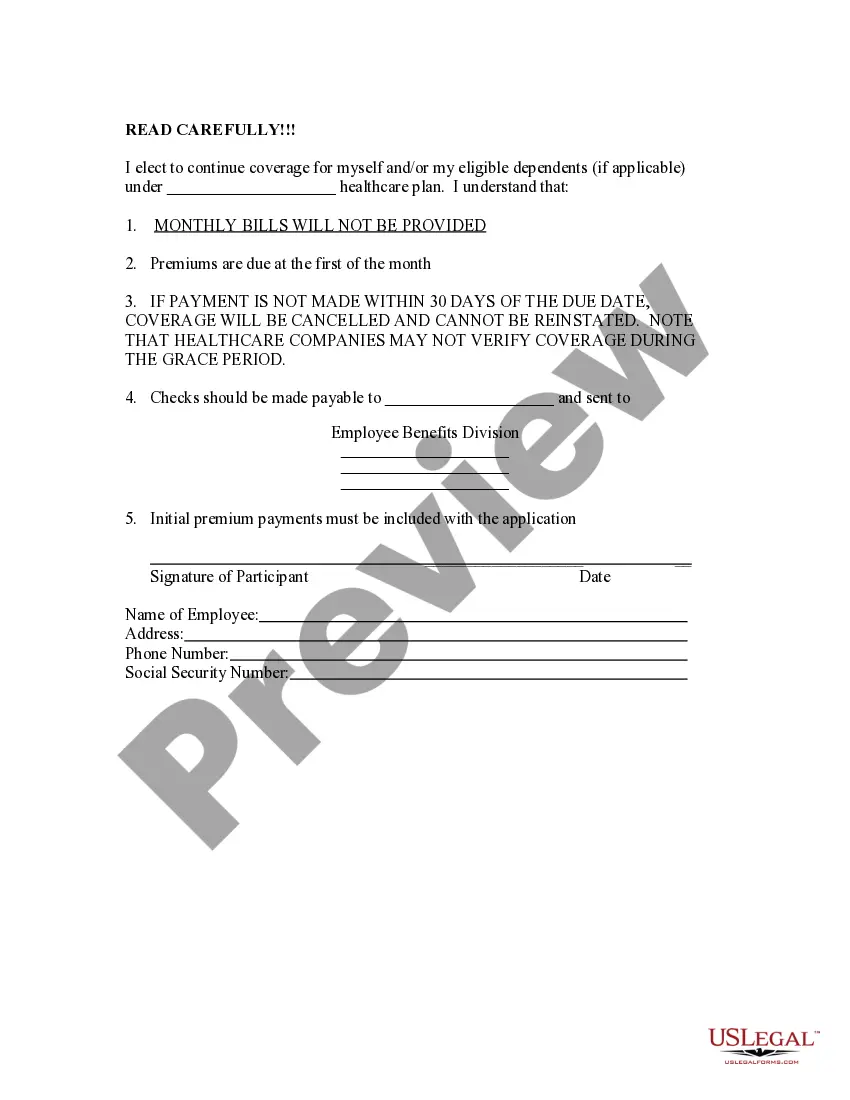
The Bexar Texas Election Form for Continuation of Benefits, also known as COBRA (Consolidated Omnibus Budget Reconciliation Act), is a crucial document that enables eligible employees to continue their health insurance coverage after experiencing a qualifying event that would otherwise result in the loss of benefits. COBRA gives individuals the opportunity to maintain their existing health insurance coverage for a temporary period, ensuring they do not face a disruption in healthcare services during times of transition. The Bexar Texas Election Form for Continuation of Benefits — COBRA outlines the necessary steps and information needed to exercise this option. When employees become eligible for COBRA in Bexar Texas, there are several types of Election Forms they may encounter, depending on their specific circumstances. These different forms might include: 1. Initial Election Form: This form is used when an employee or their eligible dependents initially become eligible for COBRA benefits due to the occurrence of a qualifying event, such as termination, reduction of hours, or death of the covered employee. 2. Open Enrollment Election Form: Employees who have previously elected COBRA coverage and are still within their COBRA coverage period may have the opportunity to make changes to their existing coverage during open enrollment periods. The Open Enrollment Election Form allows them to adjust their benefits or add or remove eligible dependents. 3. Late Election Form: In some cases, individuals who initially declined COBRA coverage may have a second chance to elect it within a specific timeframe if they experience a qualifying event, such as divorce, legal separation, or loss of dependent status. The Late Election Form provides an avenue for these individuals to request continuation of benefits. It is important for eligible individuals to carefully review and complete the Bexar Texas Election Form for Continuation of Benefits — COBRA promptly to ensure they secure their right to continued healthcare coverage. Missing the deadline for submitting the form could result in the loss of COBRA benefits, leaving them without health insurance coverage during a critical period of transition.
Bexar Texas Election Form for Continuation of Benefits - COBRA
Description
How to fill out Bexar Texas Election Form For Continuation Of Benefits - COBRA?
If you need to find a trustworthy legal form provider to find the Bexar Election Form for Continuation of Benefits - COBRA, look no further than US Legal Forms. No matter if you need to launch your LLC business or manage your belongings distribution, we got you covered. You don't need to be well-versed in in law to locate and download the needed template.
- You can browse from over 85,000 forms arranged by state/county and situation.
- The intuitive interface, variety of learning materials, and dedicated support make it simple to get and execute various documents.
- US Legal Forms is a reliable service offering legal forms to millions of users since 1997.
Simply type to search or browse Bexar Election Form for Continuation of Benefits - COBRA, either by a keyword or by the state/county the document is created for. After locating needed template, you can log in and download it or save it in the My Forms tab.
Don't have an account? It's simple to start! Simply locate the Bexar Election Form for Continuation of Benefits - COBRA template and take a look at the form's preview and description (if available). If you're confident about the template’s legalese, go ahead and hit Buy now. Create an account and select a subscription option. The template will be instantly ready for download as soon as the payment is completed. Now you can execute the form.
Handling your legal affairs doesn’t have to be pricey or time-consuming. US Legal Forms is here to demonstrate it. Our comprehensive variety of legal forms makes this experience less costly and more reasonably priced. Set up your first company, arrange your advance care planning, create a real estate contract, or execute the Bexar Election Form for Continuation of Benefits - COBRA - all from the comfort of your sofa.
Join US Legal Forms now!