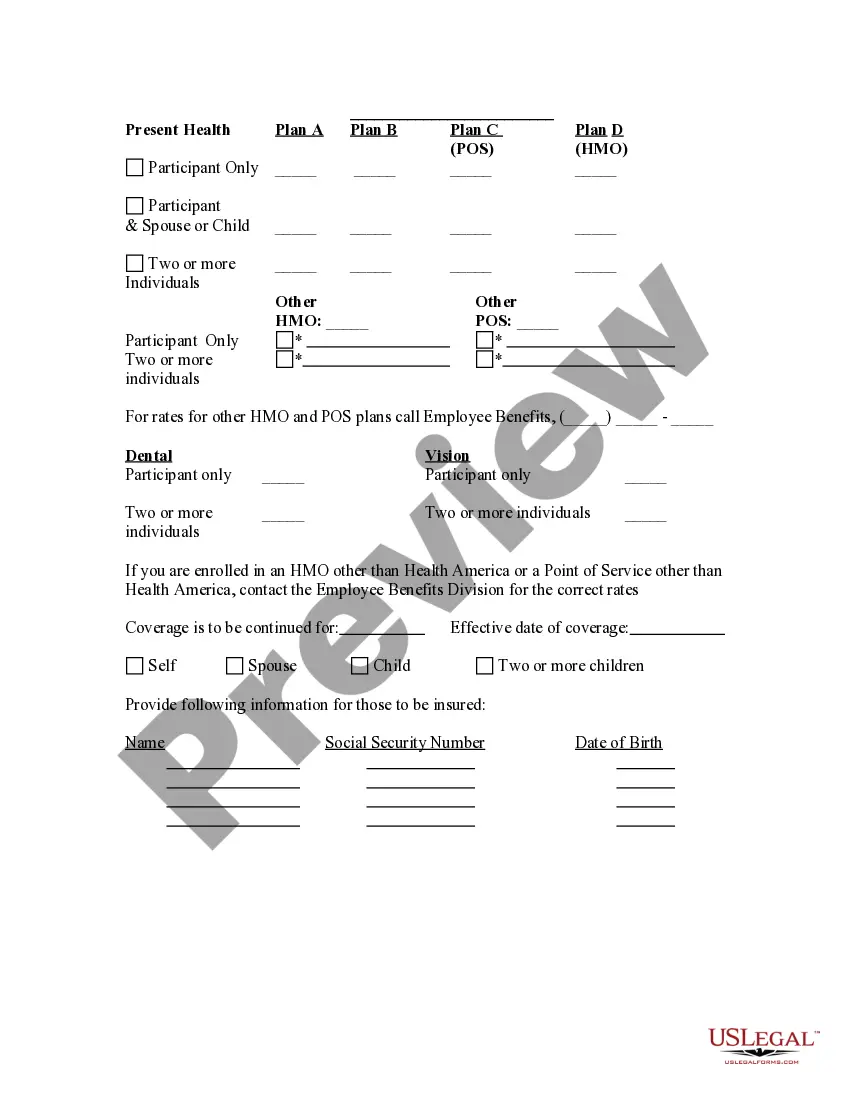
Fulton Georgia Election Form for Continuation of Benefits — COBRA is an essential document that allows eligible individuals to maintain their healthcare coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). It is important to understand the details and types of COBRA Election Forms available to ensure uninterrupted insurance coverage. The Fulton Georgia Election Form for Continuation of Benefits — COBRA must be completed by qualified individuals who have experienced qualifying events such as job loss, reduction in work hours, or other circumstances that cause a loss of employer-sponsored health benefits. This form helps individuals elect to continue their health insurance coverage by making the required premium payments. Understanding the different types of Fulton Georgia Election Forms for Continuation of Benefits — COBRA is crucial as they cater to specific situations and individuals. Here are some common types of COBRA election forms: 1. Standard COBRA Election Form: This form is typically used by employees who lose their job or have their work hours significantly reduced. It allows them to elect COBRA coverage and continue their health benefits for a limited time. 2. Spousal COBRA Election Form: In cases where a spouse loses their coverage due to a divorce or the death of the covered employee, this form enables them to elect COBRA coverage independently. 3. Dependent COBRA Election Form: This form is for dependents who lose their coverage due to reasons such as aging out of parent's insurance, divorce, or death of the covered employee. It allows them to elect COBRA coverage. 4. Qualified Beneficiary COBRA Election Form: This form is designated for individuals who were covered under a group health plan but lost their coverage due to certain qualifying events, such as loss of dependent status or the covered employee becoming eligible for Medicare. 5. State Continuation COBRA Election Form: This form may be applicable in states where continuation coverage laws extend coverage beyond the federal COBRA requirements. It allows individuals to elect to continue their health benefits according to the specific state regulations. When completing the Fulton Georgia Election Form for Continuation of Benefits — COBRA, individuals should provide accurate personal information, including names, addresses, employment details, and the dates of qualifying events. This form acts as a formal request to continue coverage and should be submitted to the appropriate entity within the required time frame. Fulton Georgia residents seeking to maintain their healthcare coverage through COBRA should promptly complete the relevant election form and ensure its submission to the appropriate party. By doing so, they can secure crucial continued benefits and peace of mind during periods of transition or unexpected events affecting their insurance coverage.
Fulton Georgia Election Form for Continuation of Benefits - COBRA
Description
How to fill out Fulton Georgia Election Form For Continuation Of Benefits - COBRA?
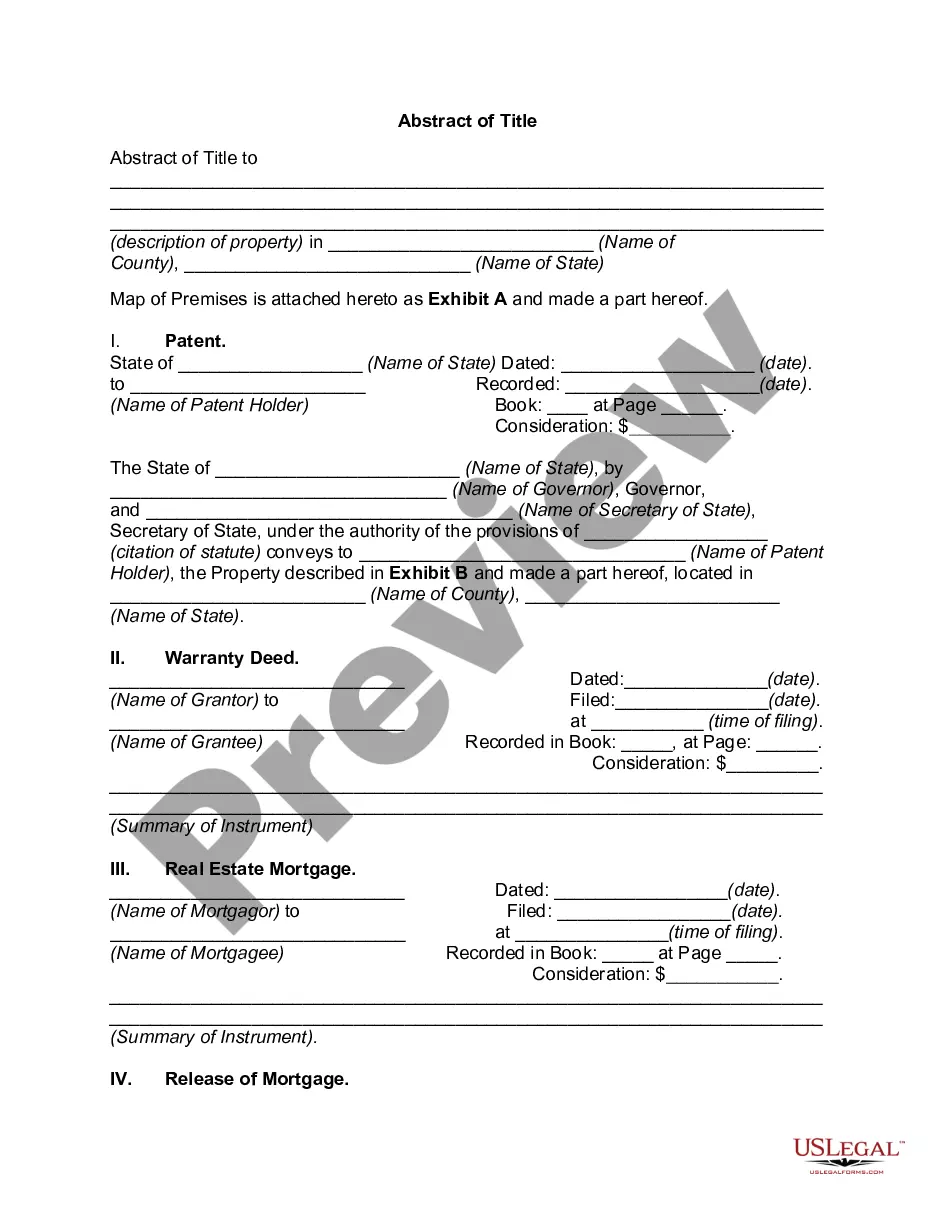
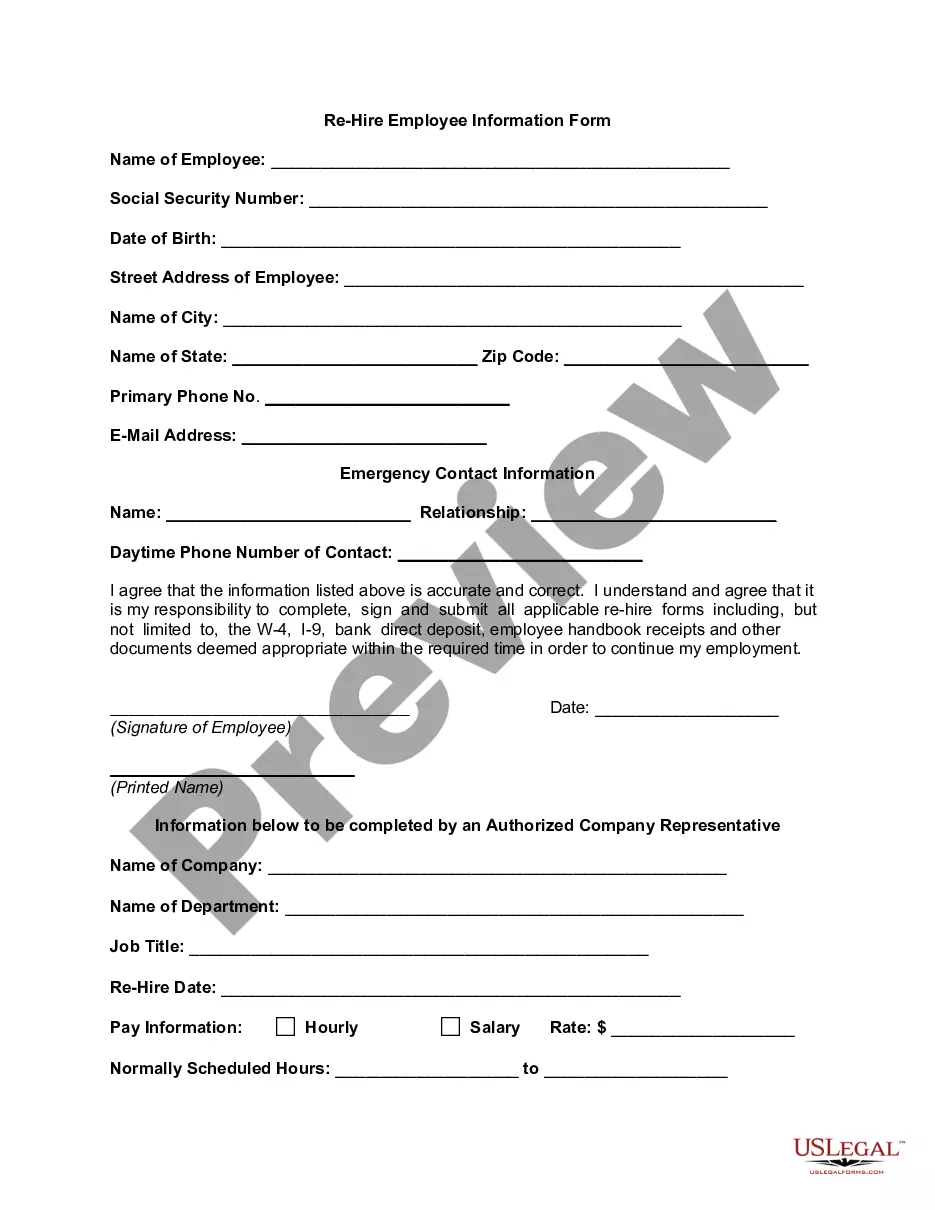
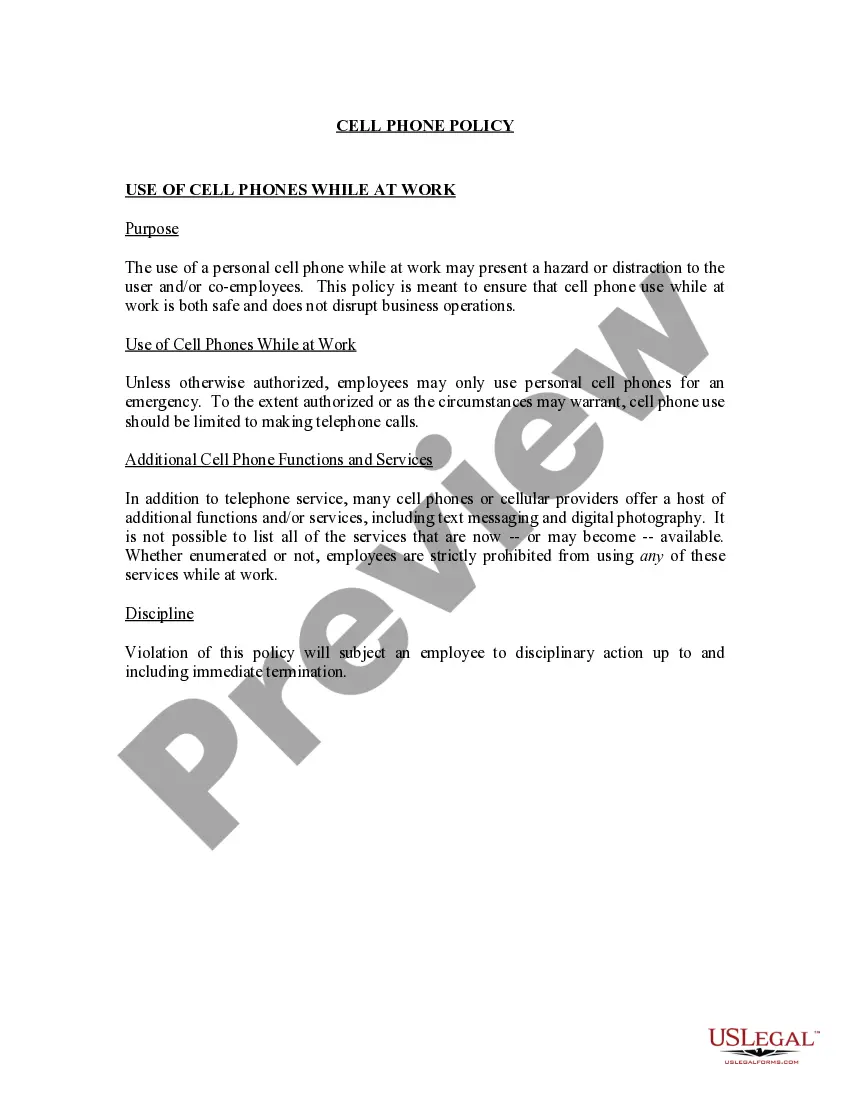
Laws and regulations in every area differ around the country. If you're not an attorney, it's easy to get lost in a variety of norms when it comes to drafting legal documents. To avoid pricey legal assistance when preparing the Fulton Election Form for Continuation of Benefits - COBRA, you need a verified template legitimate for your region. That's when using the US Legal Forms platform is so advantageous.
US Legal Forms is a trusted by millions online library of more than 85,000 state-specific legal templates. It's a great solution for specialists and individuals searching for do-it-yourself templates for various life and business scenarios. All the documents can be used many times: once you obtain a sample, it remains available in your profile for future use. Thus, if you have an account with a valid subscription, you can just log in and re-download the Fulton Election Form for Continuation of Benefits - COBRA from the My Forms tab.
For new users, it's necessary to make a few more steps to obtain the Fulton Election Form for Continuation of Benefits - COBRA:
- Examine the page content to make sure you found the correct sample.
- Take advantage of the Preview option or read the form description if available.
- Search for another doc if there are inconsistencies with any of your criteria.
- Use the Buy Now button to obtain the template once you find the right one.
- Opt for one of the subscription plans and log in or sign up for an account.
- Select how you prefer to pay for your subscription (with a credit card or PayPal).
- Pick the format you want to save the file in and click Download.
- Fill out and sign the template in writing after printing it or do it all electronically.
That's the simplest and most cost-effective way to get up-to-date templates for any legal reasons. Locate them all in clicks and keep your documentation in order with the US Legal Forms!
Form popularity
FAQ
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) health benefit provisions amend the Employee Retirement Income Security Act, the Internal Revenue Code and the Public Health Service Act to require group health plans to provide a temporary continuation of group health coverage that otherwise might be
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
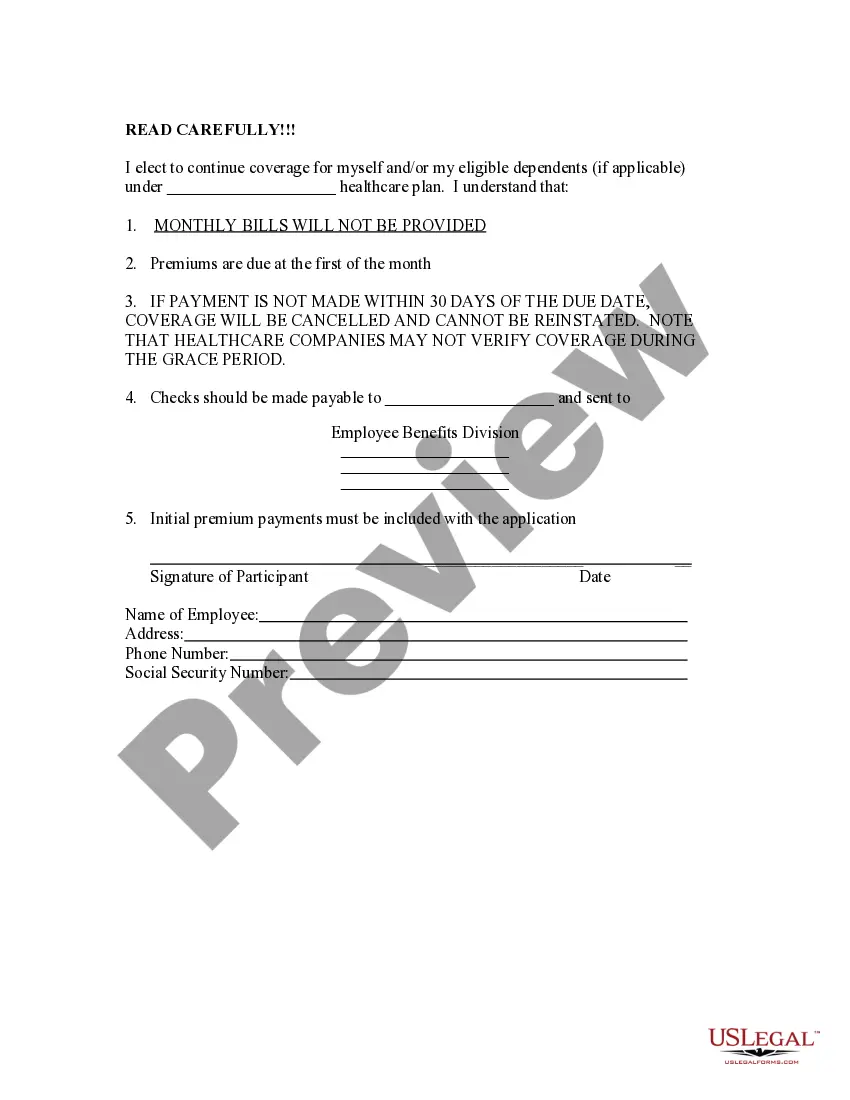
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
COBRA Election Notice The election notice describes their rights to continuation coverage and how to make an election. The election notice should include: 2022 The name of the plan and the name, address, and telephone number of the plan's COBRA.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
COBRA Election Form ("Form") The Employee should write the information of the member(s) to be covered under the COBRA policy. For COBRA coverage, Vantage must receive a copy of this Form within 60 days from the qualifying event.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,