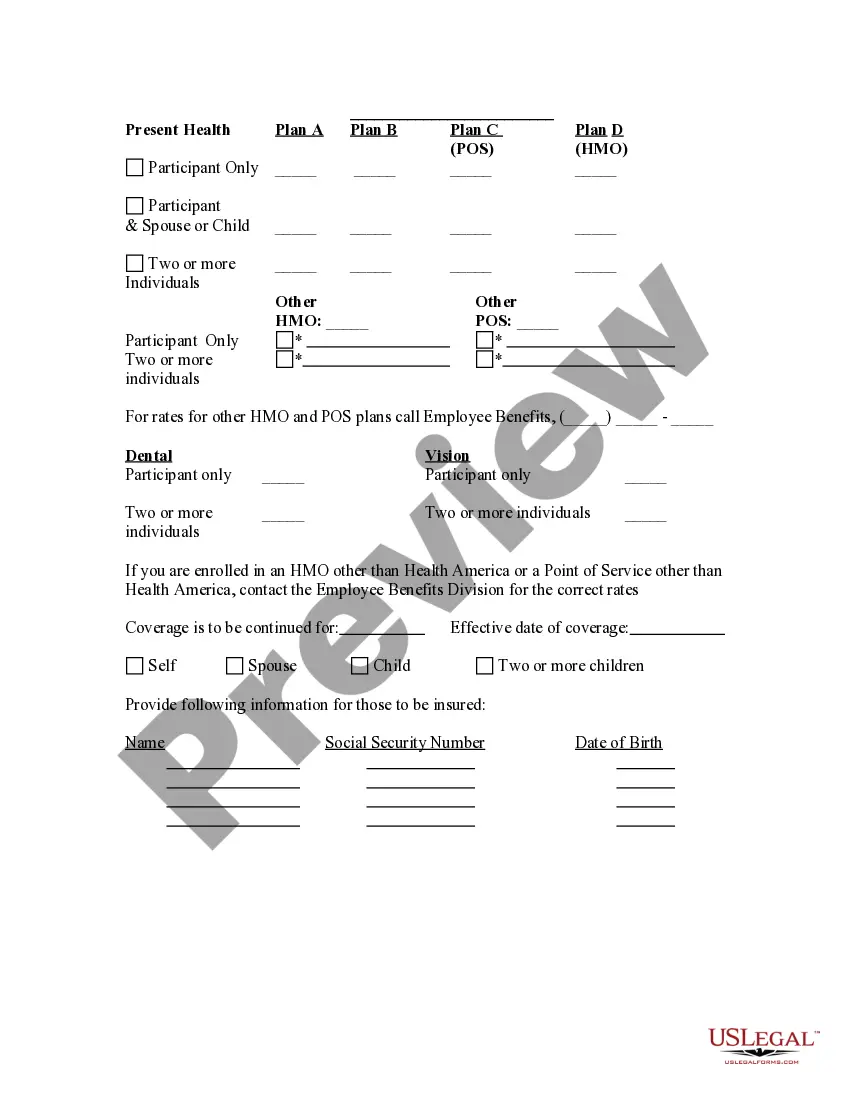
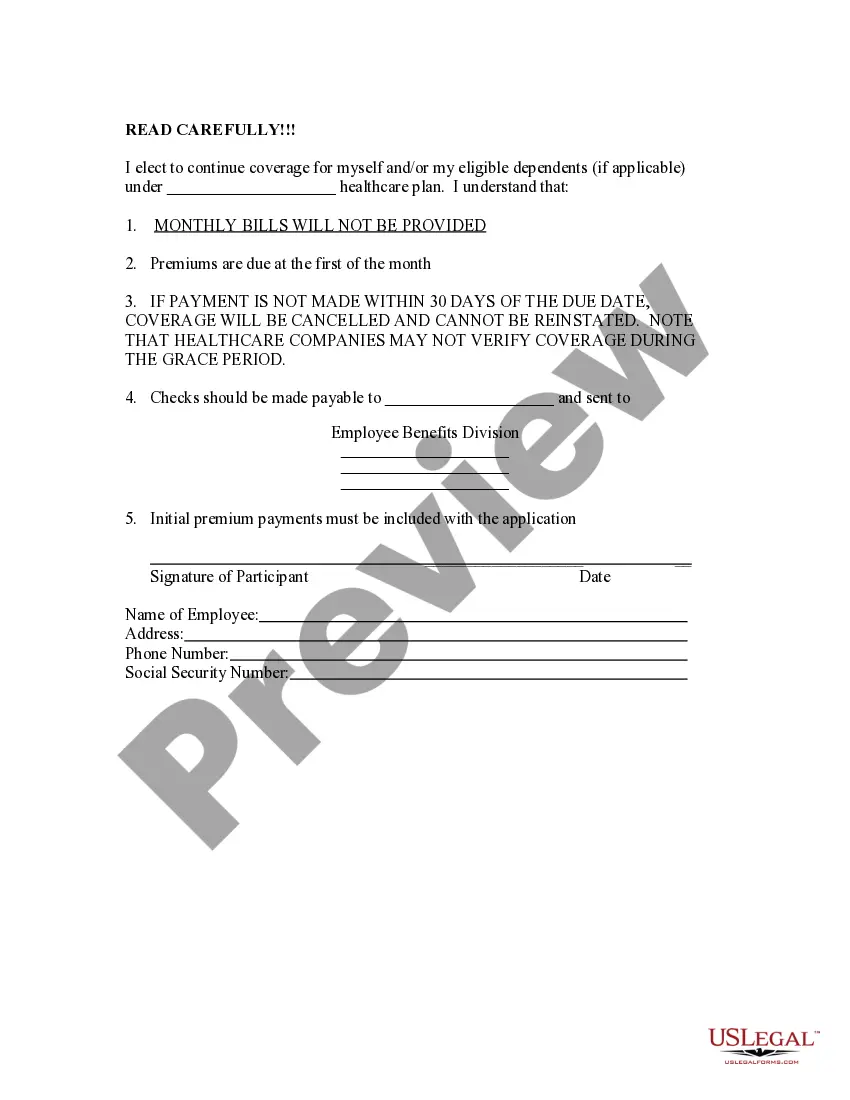
The Hillsborough Florida Election Form for Continuation of Benefits — COBRA is an essential document that allows individuals to continue their employer-provided health insurance coverage through the COBRA program. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act, which grants eligible employees the right to maintain their health insurance benefits for a specified period after certain qualifying events such as termination, reduction in hours, or divorce. This Hillsborough County-specific form is tailored to residents in Florida's Hillsborough County who are seeking to elect COBRA continuation coverage. By completing this form, individuals can ensure that they maintain access to healthcare services, prescription medications, and other medical benefits that were previously provided through their employer. The Hillsborough Florida Election Form for Continuation of Benefits — COBRA requires several key pieces of information to be filled out accurately. The form may require the following details: 1. Personal information: Full name, address, phone number, and Social Security number of the individual requesting COBRA continuation coverage. 2. Employment information: Details of the previous employer, such as the company name, address, and contact information. This information helps ensure that the individual was covered under a qualified health plan before experiencing a qualifying event. 3. Qualifying event details: The specific reason for the loss of coverage, including the date on which the qualifying event occurred. Examples of qualifying events include termination, reduction of work hours, or a dependent child reaching the age limit for coverage. 4. Coverage election: The individual should clearly indicate their election regarding continuation coverage, specifying if they wish to extend coverage for themselves, their spouse, or dependents. Different elections may require separate forms and documentation. 5. Payment information: COBRA coverage usually involves a monthly premium payment, and the form may require payment details such as preferred payment method, banking information, or authorization for payroll deduction if applicable. It's important to note that while the Hillsborough Florida Election Form for Continuation of Benefits — COBRA is the standard form used in Hillsborough County, other counties in Florida or other states may have their own variations. Therefore, individuals seeking COBRA continuation coverage should always ensure they are using the correct form specific to their location. By providing accurate and complete information on the Hillsborough Florida Election Form for Continuation of Benefits — COBRA, individuals can take the necessary steps to maintain their health insurance coverage and protect themselves and their loved ones during periods of transition or uncertainty.
Hillsborough Florida Election Form for Continuation of Benefits - COBRA
Description
How to fill out Hillsborough Florida Election Form For Continuation Of Benefits - COBRA?
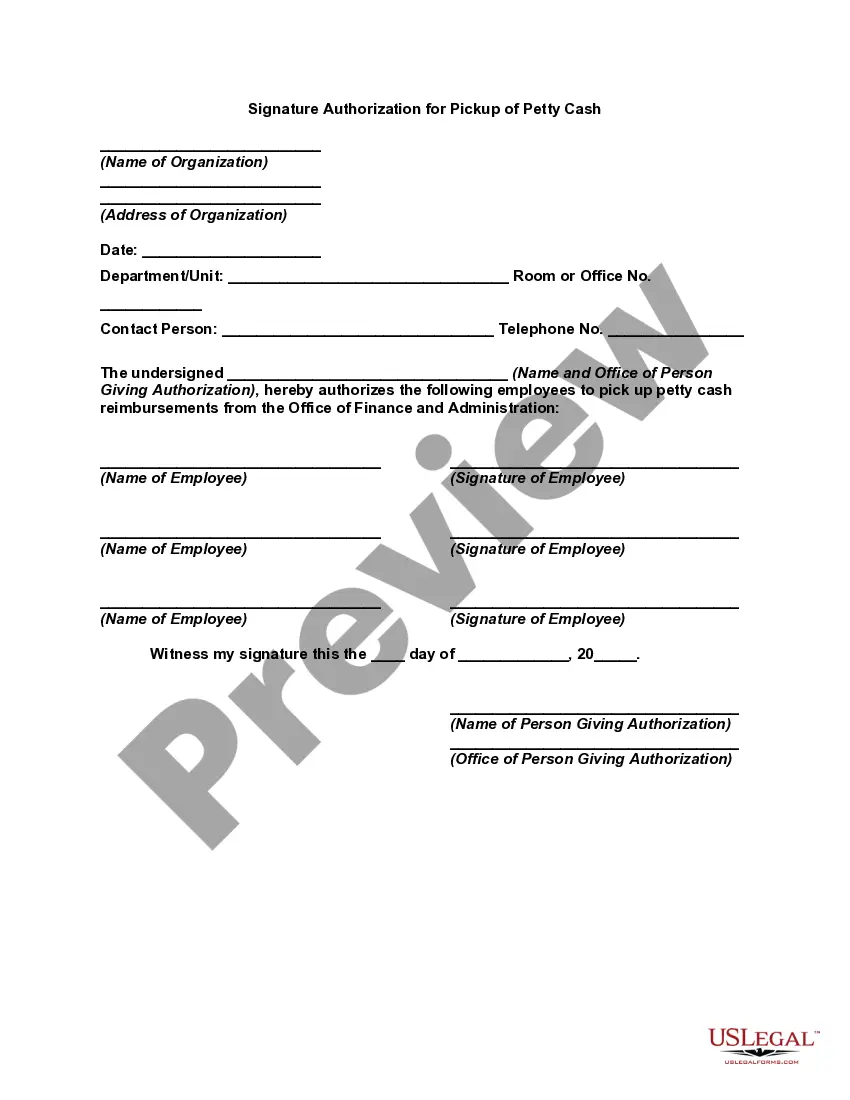
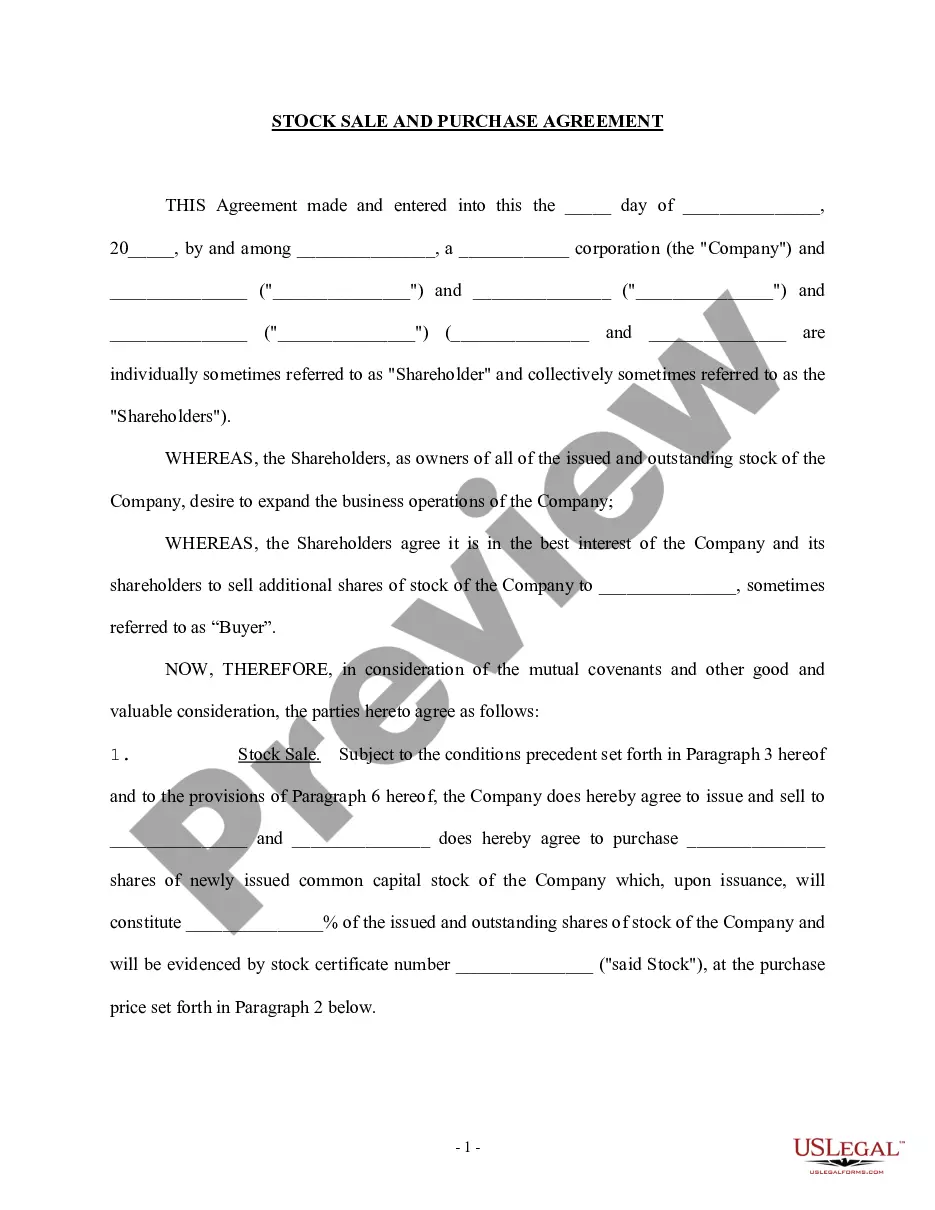
Laws and regulations in every sphere differ around the country. If you're not a lawyer, it's easy to get lost in a variety of norms when it comes to drafting legal paperwork. To avoid high priced legal assistance when preparing the Hillsborough Election Form for Continuation of Benefits - COBRA, you need a verified template legitimate for your region. That's when using the US Legal Forms platform is so beneficial.
US Legal Forms is a trusted by millions online catalog of more than 85,000 state-specific legal templates. It's an excellent solution for professionals and individuals looking for do-it-yourself templates for various life and business situations. All the documents can be used multiple times: once you obtain a sample, it remains accessible in your profile for future use. Therefore, if you have an account with a valid subscription, you can just log in and re-download the Hillsborough Election Form for Continuation of Benefits - COBRA from the My Forms tab.
For new users, it's necessary to make a couple of more steps to obtain the Hillsborough Election Form for Continuation of Benefits - COBRA:
- Examine the page content to make sure you found the right sample.
- Utilize the Preview option or read the form description if available.
- Look for another doc if there are inconsistencies with any of your criteria.
- Utilize the Buy Now button to get the template when you find the right one.
- Opt for one of the subscription plans and log in or sign up for an account.
- Decide how you prefer to pay for your subscription (with a credit card or PayPal).
- Pick the format you want to save the document in and click Download.
- Fill out and sign the template on paper after printing it or do it all electronically.
That's the simplest and most cost-effective way to get up-to-date templates for any legal reasons. Locate them all in clicks and keep your documentation in order with the US Legal Forms!
Form popularity
FAQ
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
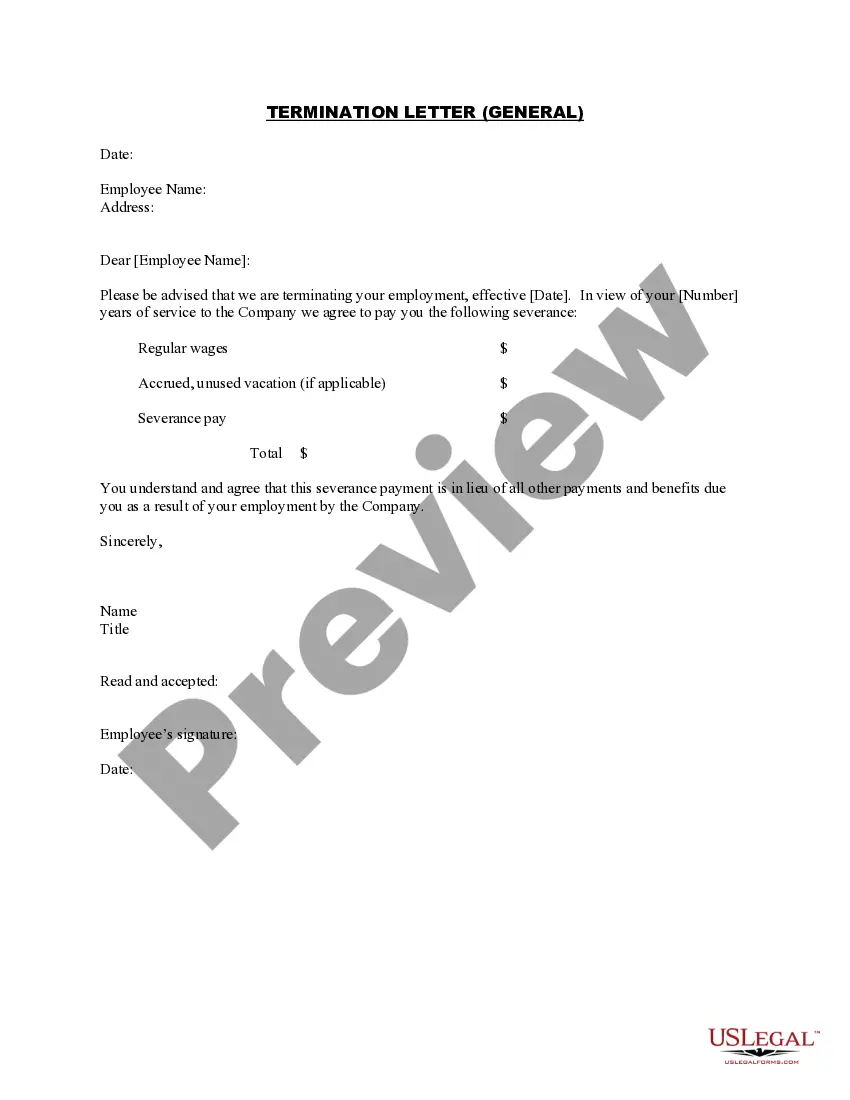
COBRA Election Form ("Form") The Employee should write the information of the member(s) to be covered under the COBRA policy. For COBRA coverage, Vantage must receive a copy of this Form within 60 days from the qualifying event.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
COBRA Election Notice The election notice describes their rights to continuation coverage and how to make an election. The election notice should include: 2022 The name of the plan and the name, address, and telephone number of the plan's COBRA.
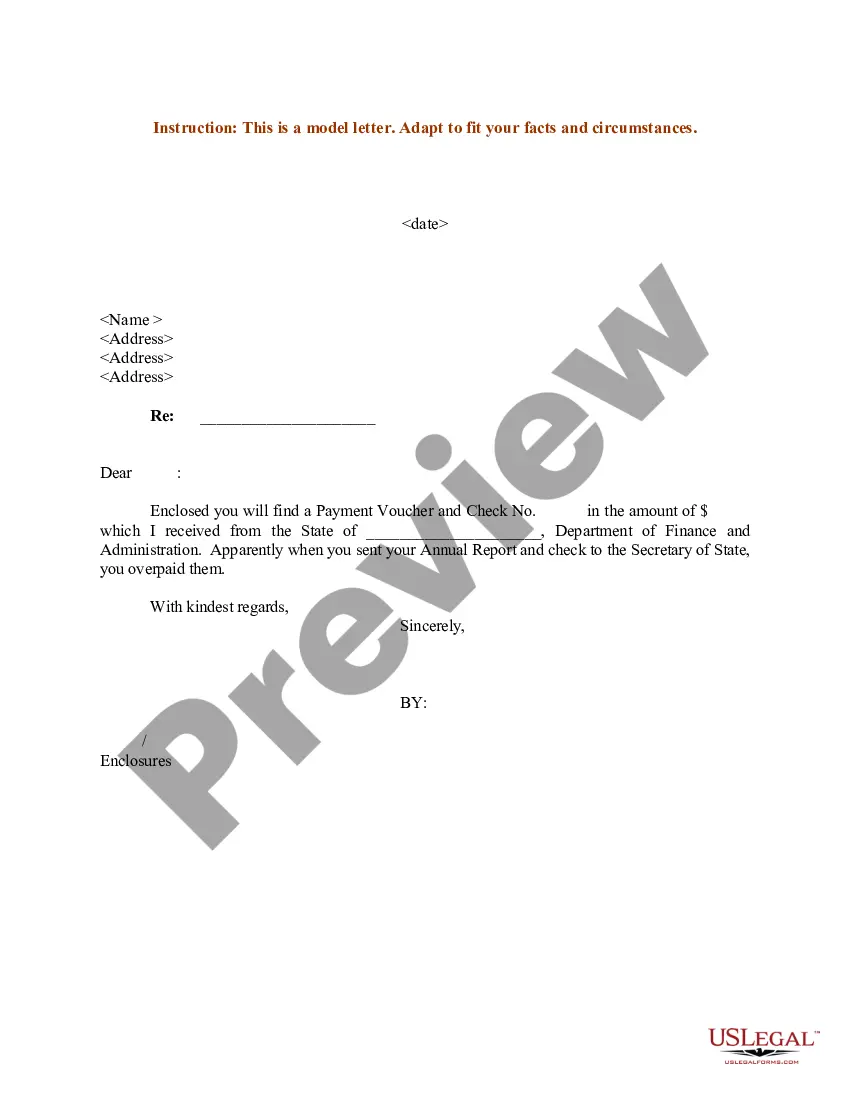
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) health benefit provisions amend the Employee Retirement Income Security Act, the Internal Revenue Code and the Public Health Service Act to require group health plans to provide a temporary continuation of group health coverage that otherwise might be
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
For covered employees, the only qualifying event is termination of employment (whether the termination is voluntary or involuntary) including by retirement, or reduction of employment hours. In that case, COBRA lasts for eighteen months.
More info
What's Included? Chapter One — How Is My Plan Composed? Chapter Two — How Does My Plan Pay? Chapter Three — How Does It Do It? Chapter Four — When Do Benefits Begin? Chapter Five — What Benefits Do I Get? Chapter Six — How Long Do I Receive Benefits After I Leave the Plan? Chapter Seven — Do I Have to Pay Tax on Benefits? Chapter Eight — Are Other Carriers of Insurance Offered in My Area? What You Will Read In this chapter you will learn about: Who Is Covered By Medicare Advantage? What Kind of Coverage is Available? Who Can Apply? Who Is Eligible to Applies What Is the Plan Structure? What Is Medicare Advantage? What Is the Medicare Advantage Benefits? A brief history of the Medicare Advantage program. What's New in the new Medicare Advantage plan: How Medicare has expanded its benefit program. How Medicare pays for Medicare Advantage plans This overview of the program tells you all about whose covered by Medicare Advantage plans.
Disclaimer
The materials in this section are taken from public sources. We disclaim all representations or any warranties, express or implied, as to the accuracy, authenticity, reliability, accessibility, adequacy, or completeness of any data in this paragraph. Nevertheless, we make every effort to cite public sources deemed reliable and trustworthy.