Broward Florida Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
Preparing documents for the business or personal requirements is always a significant obligation.
When formulating a contract, a public service application, or a power of attorney, it's vital to take into account all federal and state regulations of the particular area.
Nonetheless, small counties and even municipalities also have legislative rules that you need to be aware of.
The remarkable aspect of the US Legal Forms library is that all the documents you've ever obtained remain accessible - you can find them in your profile under the My documents tab at any time. Join the platform and easily acquire validated legal forms for any purpose with just a few clicks!
- All these factors render it challenging and time-intensive to compose a Broward Introductory COBRA Letter without expert assistance.
- It's simple to avoid squandering funds on lawyers drafting your documents and to produce a legally sound Broward Introductory COBRA Letter independently, utilizing the US Legal Forms online repository.
- It is the largest online collection of state-specific legal documents that have been professionally verified, ensuring their legality when selecting a template for your county.
- Previous subscribers only need to Log In to their accounts to retrieve the necessary form.
- If you don't yet have a subscription, follow the step-by-step instructions below to acquire the Broward Introductory COBRA Letter.
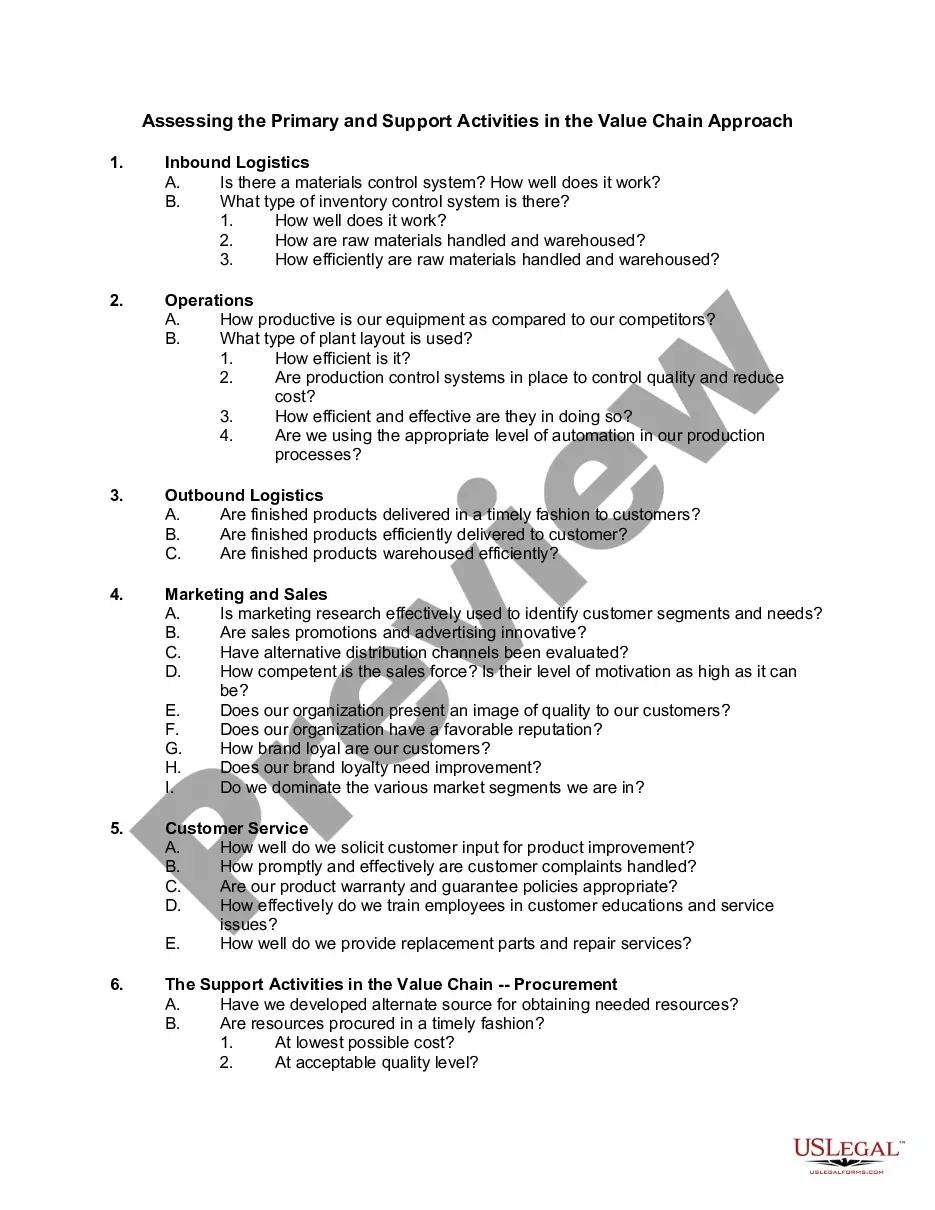
- Review the webpage you've accessed and confirm if it contains the sample you need.
- To do this, utilize the form description and preview if such features are present.
Form popularity
FAQ
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
General Notice/Initial Notice. The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan.
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or