Middlesex Massachusetts Introductory COBRA Letter serves as a vital communication document that provides important information about continuing healthcare coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). This letter is typically sent by employers to help to transition employees and their dependents understand their rights and options after a qualifying event, such as job loss or a reduction in work hours. Keywords: Middlesex Massachusetts, Introductory COBRA Letter, healthcare coverage, COBRA, communication document, employers, transitioning employees, dependents, qualifying event, job loss, reduction in work hours. Different types of Middlesex Massachusetts Introductory COBRA Letters: 1. Middlesex Massachusetts Introductory COBRA Termination Letter: This type of letter is sent when an employer cancels an employee's healthcare coverage under COBRA due to reasons such as failure to pay premiums or obtaining new group health insurance. 2. Middlesex Massachusetts Introductory COBRA Eligibility Letter: This letter notifies employees and their dependents about their initial eligibility for continuing healthcare coverage under COBRA after a qualifying event. 3. Middlesex Massachusetts Introductory COBRA Extension Letter: This letter informs employees and dependents of an extension for their current COBRA coverage period, typically due to certain circumstances like disability, second qualifying events, or other regulatory changes. 4. Middlesex Massachusetts Introductory COBRA Rights and Options Letter: This document provides a detailed explanation of the rights and options available to employees and their dependents regarding COBRA coverage, including cost, duration, and the process to elect or decline it. 5. Middlesex Massachusetts Introductory COBRA Notice of Termination Letter: This letter is sent to inform employees and their dependents about the end of their COBRA coverage, providing options for obtaining alternative healthcare coverage. These various types of Middlesex Massachusetts Introductory COBRA Letters ensure clear communication of vital information regarding COBRA coverage, rights, and obligations, helping employees and their dependents make informed decisions regarding their healthcare needs.
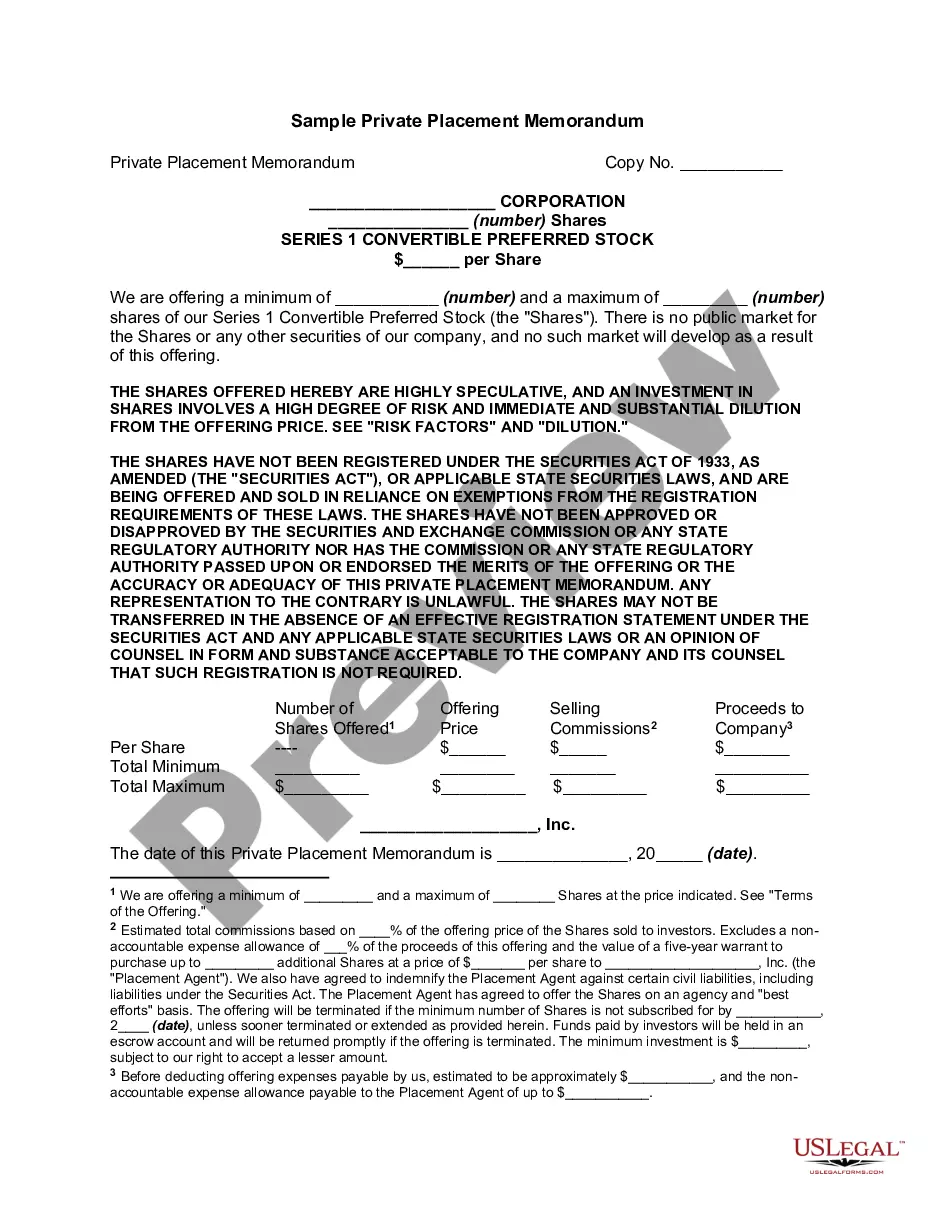
Middlesex Massachusetts Introductory COBRA Letter
Description
How to fill out Middlesex Massachusetts Introductory COBRA Letter?
Laws and regulations in every area vary throughout the country. If you're not a lawyer, it's easy to get lost in countless norms when it comes to drafting legal paperwork. To avoid costly legal assistance when preparing the Middlesex Introductory COBRA Letter, you need a verified template legitimate for your county. That's when using the US Legal Forms platform is so helpful.
US Legal Forms is a trusted by millions web collection of more than 85,000 state-specific legal forms. It's an excellent solution for specialists and individuals looking for do-it-yourself templates for different life and business scenarios. All the documents can be used many times: once you pick a sample, it remains accessible in your profile for further use. Therefore, if you have an account with a valid subscription, you can simply log in and re-download the Middlesex Introductory COBRA Letter from the My Forms tab.
For new users, it's necessary to make some more steps to get the Middlesex Introductory COBRA Letter:
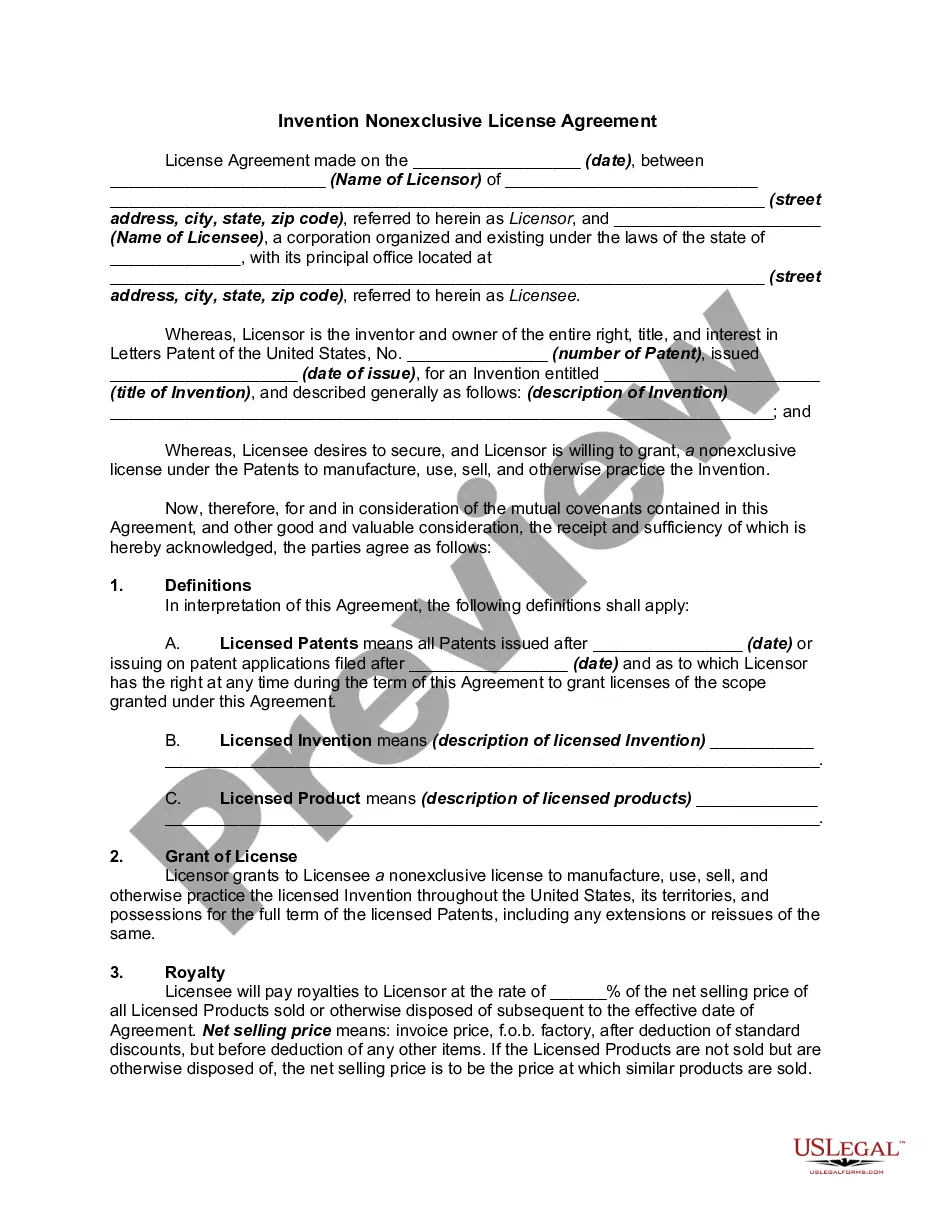
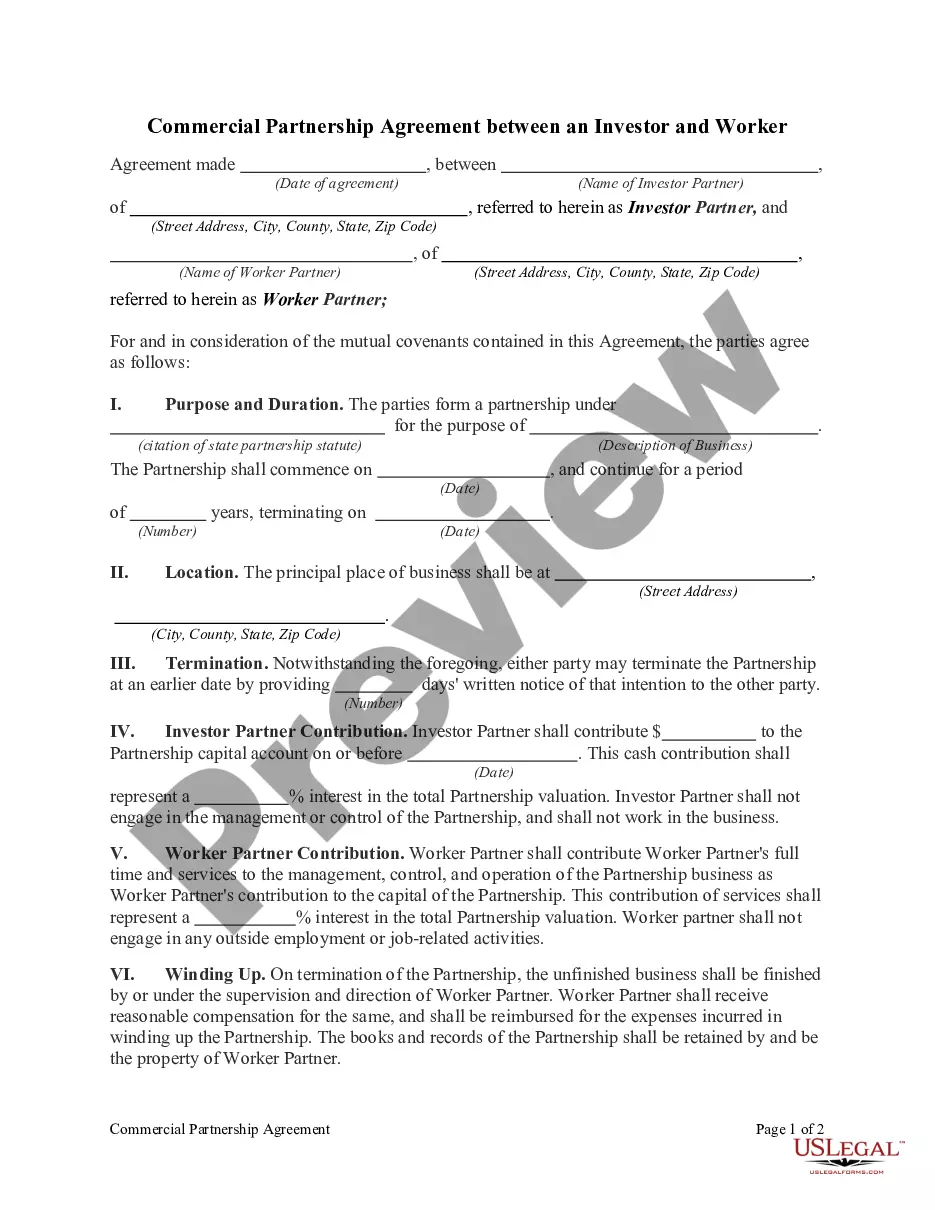
- Take a look at the page content to ensure you found the right sample.
- Utilize the Preview option or read the form description if available.
- Look for another doc if there are inconsistencies with any of your requirements.
- Use the Buy Now button to obtain the document when you find the proper one.
- Choose one of the subscription plans and log in or create an account.
- Select how you prefer to pay for your subscription (with a credit card or PayPal).
- Select the format you want to save the document in and click Download.
- Complete and sign the document in writing after printing it or do it all electronically.
That's the simplest and most affordable way to get up-to-date templates for any legal reasons. Find them all in clicks and keep your documentation in order with the US Legal Forms!