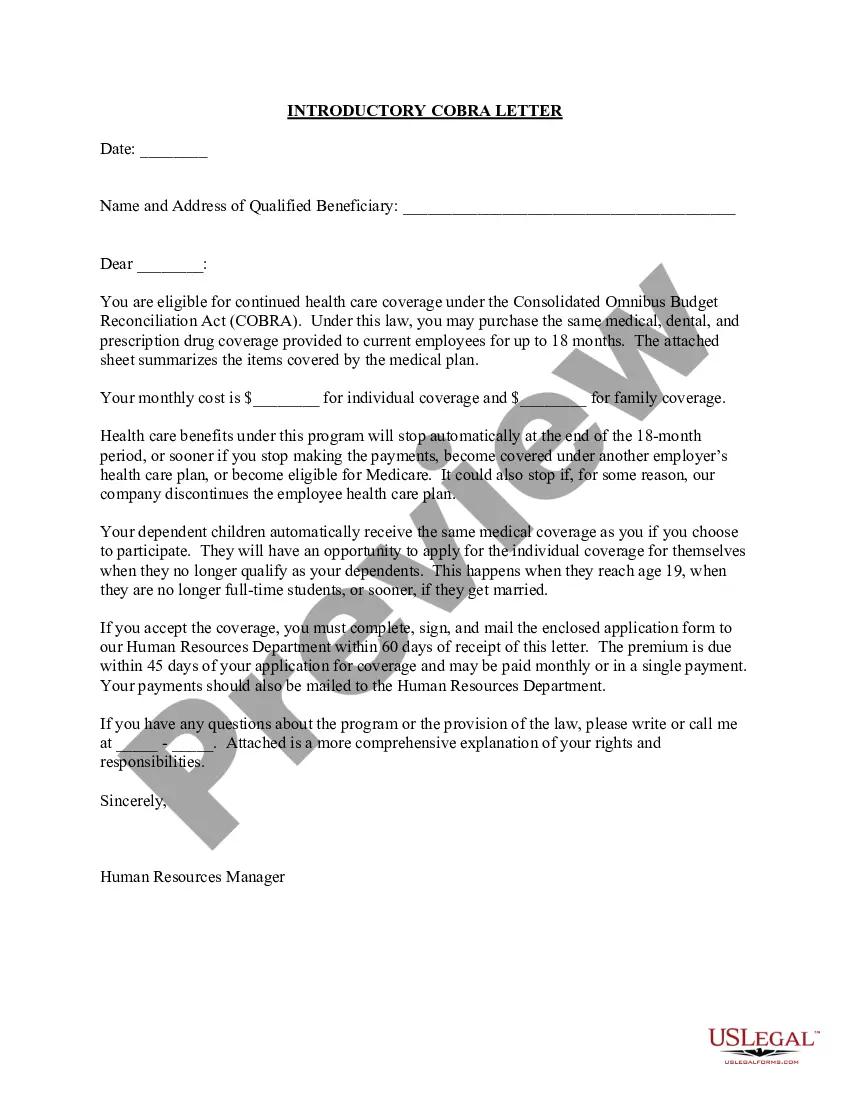
A Phoenix Arizona Introductory COBRA Letter is a document that serves as an introduction to the COBRA (Consolidated Omnibus Budget Reconciliation Act) coverage options provided to employees who have experienced a qualifying event that triggers their eligibility for continued health insurance coverage. The purpose of the Phoenix Arizona Introductory COBRA Letter is to inform the employee about their rights and responsibilities under COBRA, including the option to continue their health insurance coverage for a certain period of time. This letter is typically sent by the employer or the health insurance plan administrator, and it must be provided within specific timeframes after the qualifying event has occurred. Important keywords related to this topic include: 1. Phoenix Arizona: Refers to the location where the COBRA coverage is being offered. Phoenix is the capital city of Arizona and a major metropolitan area. 2. Introductory: Indicates that the letter is being sent at the beginning of the COBRA coverage process. 3. COBRA Letter: Denotes the type of communication being sent to the employee regarding their COBRA benefits. Types of Phoenix Arizona Introductory COBRA Letters may include: 1. Qualifying Event Notification: This type of letter is sent to an employee or covered dependent to inform them that a qualifying event has occurred, such as termination of employment, reduction in work hours, divorce, or death of the covered employee. It explains their eligibility for COBRA coverage and provides instructions on how to enroll. 2. Rights and Responsibilities: This type of letter outlines the rights and responsibilities of the employee or covered dependent regarding their COBRA coverage. It highlights the duration of coverage, premium payment obligations, and consequences for failure to comply. 3. Premium and Enrollment Details: This type of letter provides specific information about the premium amounts, payment due dates, and options for enrolling in COBRA coverage. It may include instructions for completing enrollment forms or contacting the plan administrator. 4. Transition to COBRA: This type of letter is sent to employees who have recently become eligible for COBRA coverage. It explains the process of transitioning from their previous group health insurance plan to COBRA and the steps they need to take to ensure continuous coverage. In conclusion, a Phoenix Arizona Introductory COBRA Letter is a crucial document that informs employees and their dependents about their rights and options under COBRA. It varies in format and content depending on the specific purpose of the communication, such as qualifying event notification, rights and responsibilities, premium and enrollment details, or transition instructions.
Phoenix Arizona Introductory COBRA Letter
Description
How to fill out Phoenix Arizona Introductory COBRA Letter?
Whether you intend to open your business, enter into a contract, apply for your ID renewal, or resolve family-related legal concerns, you must prepare certain documentation corresponding to your local laws and regulations. Finding the right papers may take a lot of time and effort unless you use the US Legal Forms library.
The service provides users with more than 85,000 expertly drafted and checked legal documents for any personal or business occasion. All files are collected by state and area of use, so opting for a copy like Phoenix Introductory COBRA Letter is quick and straightforward.
The US Legal Forms website users only need to log in to their account and click the Download key next to the required template. If you are new to the service, it will take you a few additional steps to get the Phoenix Introductory COBRA Letter. Follow the guidelines below:
- Make sure the sample fulfills your individual needs and state law requirements.
- Look through the form description and check the Preview if there’s one on the page.
- Utilize the search tab providing your state above to find another template.
- Click Buy Now to obtain the sample once you find the proper one.
- Opt for the subscription plan that suits you most to continue.
- Sign in to your account and pay the service with a credit card or PayPal.
- Download the Phoenix Introductory COBRA Letter in the file format you require.
- Print the copy or fill it out and sign it electronically via an online editor to save time.
Documents provided by our website are multi-usable. Having an active subscription, you are able to access all of your previously acquired paperwork whenever you need in the My Forms tab of your profile. Stop wasting time on a endless search for up-to-date formal documentation. Join the US Legal Forms platform and keep your paperwork in order with the most comprehensive online form library!