The San Antonio Texas Model COBRA Continuation Coverage Election Notice is a crucial document that provides important information to eligible employees and their families regarding their rights to continue their healthcare coverage through the Consolidated Omnibus Budget Reconciliation Act (COBRA). This notice is a mandatory requirement under federal law and must be provided by employers to individuals who are eligible for COBRA coverage. The San Antonio Texas Model COBRA Continuation Coverage Election Notice outlines the key details of the COBRA program, including the rights and responsibilities of both the employee and the healthcare plan. It explains who is eligible for COBRA coverage, what events trigger eligibility (such as termination of employment, reduction in hours, or divorce), the length of coverage available, and how to elect and pay for continuation coverage. This notice also emphasizes the importance of timely responses, clarifying that eligible individuals must elect COBRA coverage within a specific timeframe to avoid losing their right to continuation coverage. It provides instructions on how to notify the plan administrator of the election, the duration of coverage available, and the applicable premium rates. In terms of different types of San Antonio Texas Model COBRA Continuation Coverage Election Notices, there may be variations based on the specifics of the employer's healthcare plan. However, these variations generally do not change the fundamental information provided in the notice or the overall requirements of the COBRA program. Some possible variations could include notices for different types of employee groups (e.g., full-time versus part-time employees), notices specific to different types of events triggering COBRA eligibility (e.g., retirement versus termination of employment), or notices tailored to the specific healthcare plan options available to eligible individuals. Overall, the San Antonio Texas Model COBRA Continuation Coverage Election Notice is a vital document that ensures eligible employees and their families are fully aware of their rights and options regarding the continuation of healthcare coverage. It serves as a resource for navigating the COBRA program and safeguarding individuals' access to crucial healthcare services during transitional periods.
San Antonio Texas Model COBRA Continuation Coverage Election Notice
Description
How to fill out San Antonio Texas Model COBRA Continuation Coverage Election Notice?
How much time does it normally take you to draw up a legal document? Given that every state has its laws and regulations for every life situation, locating a San Antonio Model COBRA Continuation Coverage Election Notice meeting all local requirements can be tiring, and ordering it from a professional attorney is often expensive. Numerous online services offer the most popular state-specific documents for download, but using the US Legal Forms library is most beneficial.
US Legal Forms is the most extensive online catalog of templates, grouped by states and areas of use. Aside from the San Antonio Model COBRA Continuation Coverage Election Notice, here you can find any specific document to run your business or personal affairs, complying with your regional requirements. Experts check all samples for their validity, so you can be certain to prepare your paperwork correctly.
Using the service is fairly simple. If you already have an account on the platform and your subscription is valid, you only need to log in, pick the required sample, and download it. You can pick the document in your profile at any time in the future. Otherwise, if you are new to the platform, there will be some extra actions to complete before you get your San Antonio Model COBRA Continuation Coverage Election Notice:
- Check the content of the page you’re on.
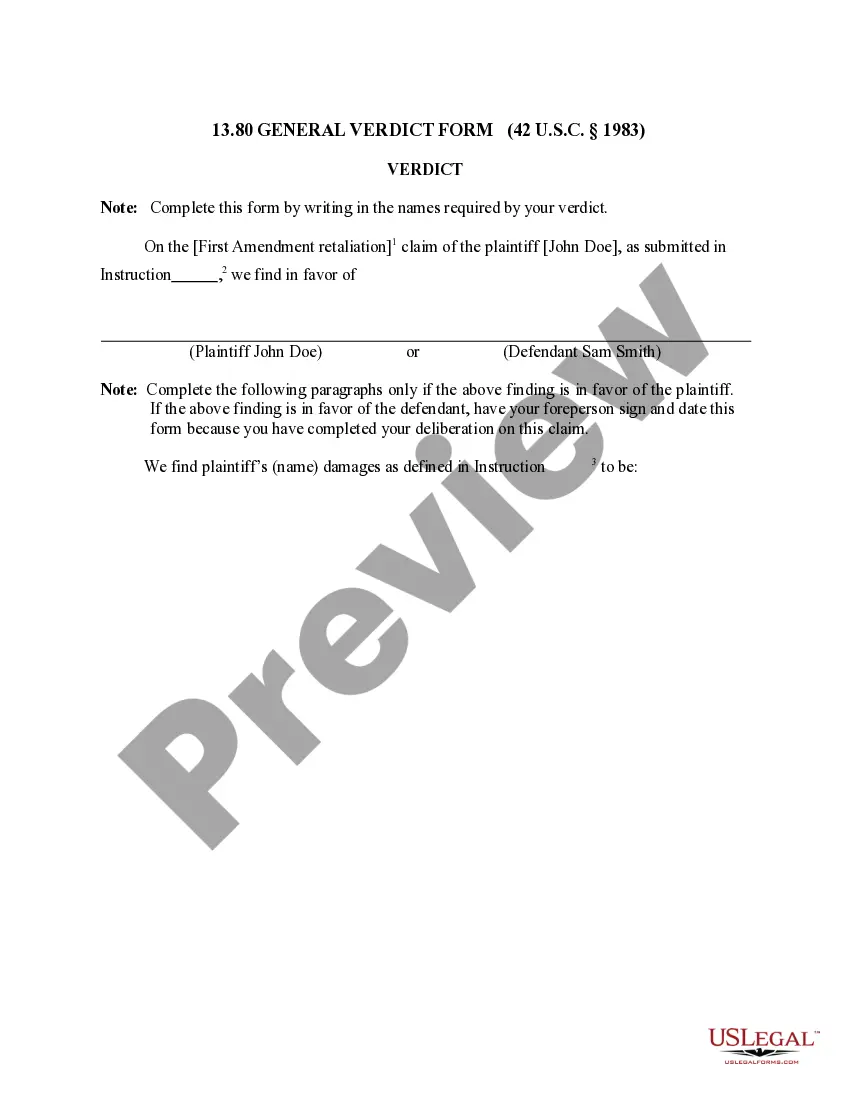
- Read the description of the sample or Preview it (if available).
- Search for another document utilizing the related option in the header.
- Click Buy Now once you’re certain in the chosen document.
- Decide on the subscription plan that suits you most.
- Sign up for an account on the platform or log in to proceed to payment options.
- Make a payment via PalPal or with your credit card.
- Switch the file format if needed.
- Click Download to save the San Antonio Model COBRA Continuation Coverage Election Notice.
- Print the sample or use any preferred online editor to complete it electronically.
No matter how many times you need to use the acquired template, you can find all the samples you’ve ever downloaded in your profile by opening the My Forms tab. Give it a try!