The Cuyahoga Ohio Notice of Qualifying Event is an essential document that employers must provide to their plan administrators in the case of certain life events that impact an employee's eligibility for health insurance coverage. It serves as a formal notification and prompts adjustments to the employee's health benefits accordingly. When an employee experiences a qualifying event, such as marriage, divorce, birth of a child, adoption, or loss of coverage, the employer must promptly notify the plan administrator via the Cuyahoga Ohio Notice of Qualifying Event. This ensures that employees have the opportunity to make necessary changes to their health insurance coverage or enroll in a plan, as needed. There are different types of Cuyahoga Ohio Notice of Qualifying Events that an employer may encounter, depending on the circumstances. Some common examples include: 1. Marriage: If an employee gets married, they may need to add their spouse to their health insurance plan or make other adjustments to their coverage. 2. Divorce or Legal Separation: In the event of a divorce or legal separation, an employee may need to remove their ex-spouse from their health plan or secure new coverage if they were previously on their spouse's plan. 3. Birth or Adoption: When an employee welcomes a new child into their family through birth or adoption, they can notify the plan administrator to add the child to their health plan or explore other coverage options. 4. Loss of Coverage: If an employee or their dependents lose coverage due to factors like termination of employment, the expiration of COBRA benefits, or the aged-out status of dependent children, the Cuyahoga Ohio Notice of Qualifying Event is crucial in ensuring timely adjustments to health insurance coverage. These examples represent just a few instances where a Cuyahoga Ohio Notice of Qualifying Event from Employer to Plan Administrator might be required. It is important for employers and employees alike to understand the significance of promptly notifying the plan administrator in order to maintain appropriate health coverage and avoid potential gaps. Compliance with these requirements helps ensure transparency, effective communication, and the necessary adjustments to employee benefits.
Cuyahoga Ohio Notice of Qualifying Event from Employer to Plan Administrator
Description
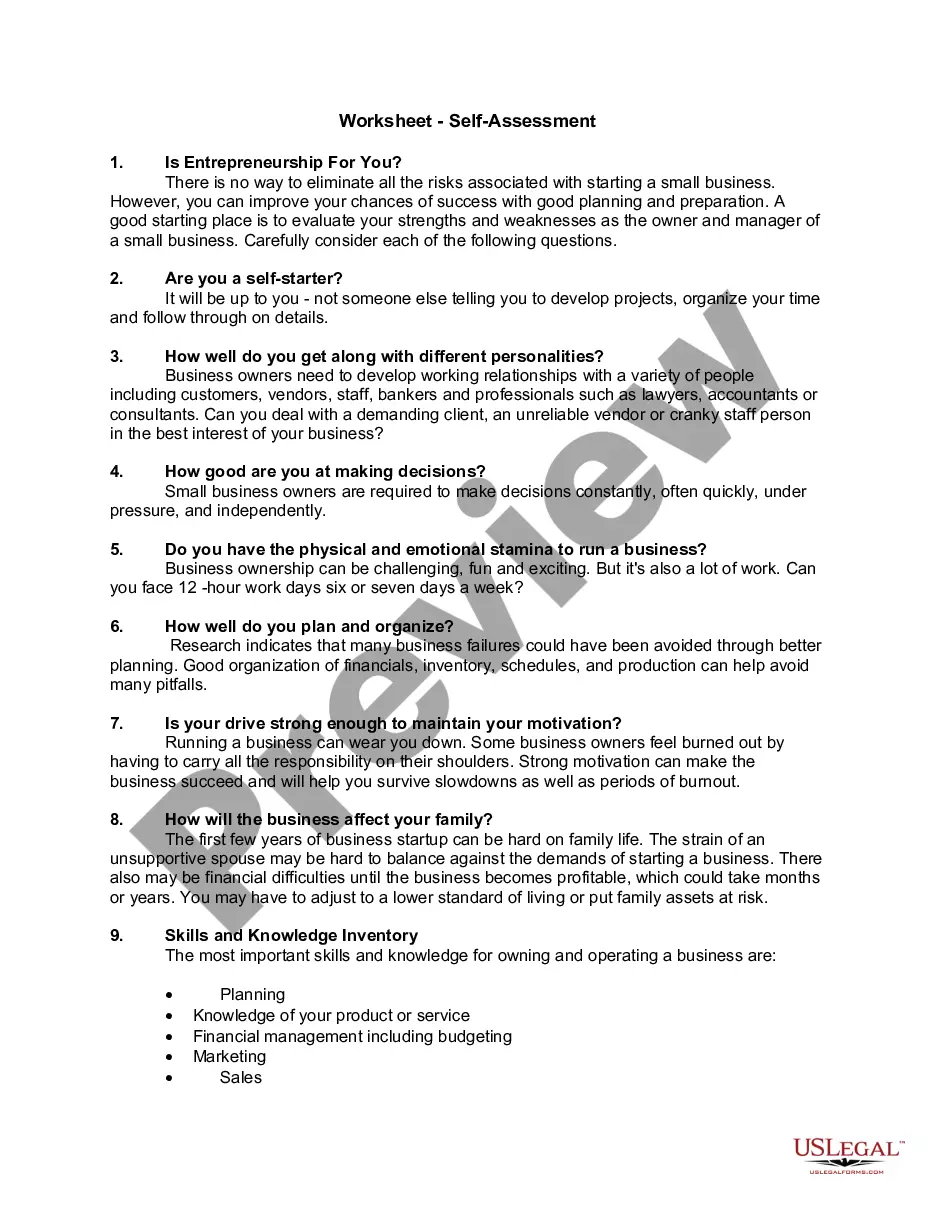
How to fill out Cuyahoga Ohio Notice Of Qualifying Event From Employer To Plan Administrator?
Laws and regulations in every area differ throughout the country. If you're not a lawyer, it's easy to get lost in a variety of norms when it comes to drafting legal documents. To avoid high priced legal assistance when preparing the Cuyahoga Notice of Qualifying Event from Employer to Plan Administrator, you need a verified template legitimate for your region. That's when using the US Legal Forms platform is so beneficial.
US Legal Forms is a trusted by millions online collection of more than 85,000 state-specific legal forms. It's a great solution for specialists and individuals searching for do-it-yourself templates for various life and business situations. All the forms can be used multiple times: once you purchase a sample, it remains available in your profile for further use. Therefore, when you have an account with a valid subscription, you can just log in and re-download the Cuyahoga Notice of Qualifying Event from Employer to Plan Administrator from the My Forms tab.
For new users, it's necessary to make some more steps to get the Cuyahoga Notice of Qualifying Event from Employer to Plan Administrator:
- Analyze the page content to make sure you found the appropriate sample.
- Utilize the Preview option or read the form description if available.
- Search for another doc if there are inconsistencies with any of your criteria.
- Utilize the Buy Now button to get the document once you find the appropriate one.
- Opt for one of the subscription plans and log in or sign up for an account.
- Select how you prefer to pay for your subscription (with a credit card or PayPal).
- Pick the format you want to save the document in and click Download.
- Complete and sign the document on paper after printing it or do it all electronically.
That's the simplest and most cost-effective way to get up-to-date templates for any legal scenarios. Locate them all in clicks and keep your paperwork in order with the US Legal Forms!